While the tumors were severely disfiguring, concern regarding the etiology of the lesions was not addressed for many years. It was not until 2015 that her pediatric surgeon noted a possible association between cyclosporine and fibroadenoma, at which point, cyclosporine was discontinued and tacrolimus initiated. There has been no further tumor recurrence since the discontinuation of cyclosporine.
Discussion
Pediatric breast disease, especially breast carcinoma, is rare. Breast cancers account for less than 1% of pediatric cancers.1 The differential diagnosis for pediatric breast lesions includes simple cysts, abscess, galactocele, fibroadenoma, juvenile papillomatosis, phyllodes tumors, and malignant neoplasm.1 As with adults, fibroadenoma are the most common benign tumors in the pediatric population.1,2,3 While phyllodes tumors account for less than 1% of pediatric breast masses, malignant phyllodes are the most common primary breast malignancy in adolescents.2
As malignant breast lesions in the pediatric population are exceedingly rare and surgical intervention may affect the developing breast, management of pediatric breast lesions differs from that of adults.1 Adenoma less than three centimeters with typical appearance on imaging can be followed at six month intervals during the first year, then one year later.1 Abnormal imaging findings include non-circumscribed margins, complex solid and cystic components, posterior acoustic shadowing, size greater than three centimeters, or serial growth and should prompt biopsy.1 Event when benign appearing on ultrasound, biopsy should be considered if the patient has a history of chest irradiation or other risk factors for cancer, concurrent cancer, or positive family history of breast cancer.1 Surgical excision is recommended for benign appearing masses that are rapidly growing or larger than five centimeters.1
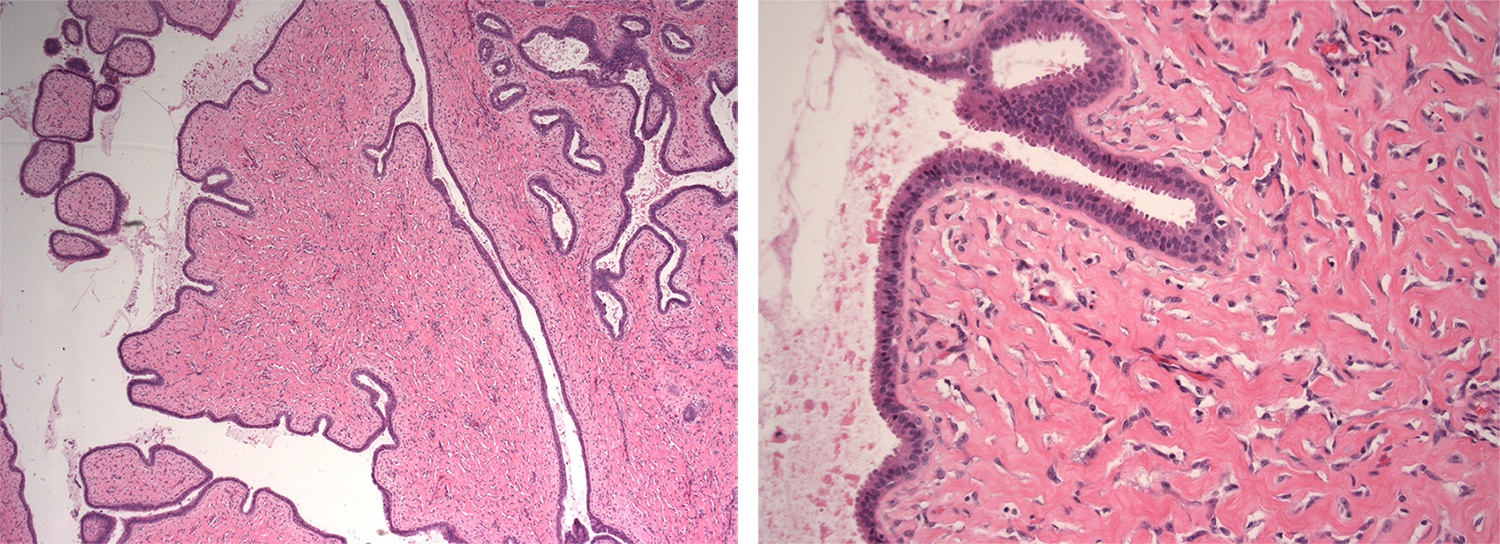
Fibroepithelial neoplasms consist of fibroadenoma and phyllodes tumors. Distinguishing cellular fibroadenoma from phyllodes tumors can be "vague and subjective" as many of these lesions have overlapping features.4 Furthermore, there is no single criterion to distinguish fibroadenoma from cellular fibroadenoma from benign phyllodes tumor.4 Treatment differs between these lesions, as well as risk of recurrence or metastasis. Risk of recurrence for phyllodes tumors increases from benign, to borderline, to malignant. As such, distinguishing the lesion is important for discussions regarding therapy and prognostic.4 A study by the Mayo Clinic found that even breast specialized pathologists disagreed on differentiating fibroadenoma from benign phyllodes, as well as subclasses of phyllodes tumors.4 Immunohistochemical markers such as Ki-67 and IMP3 have been considered to better distinguish these lesions; however, histology remains the standard of care.4,5 A diagnosis of "fibroepithelial lesions" conveys that lesions are not reproducibly distinguished between pathologists.4,6
Phyllodes tumors of the breast are a group of fibroepithelial neoplasms derived from periductal and specialized lobular stroma.6 They are classified by grade as benign, borderline, or malignant based on histology including degree of stromal cellularity and atypia, mitotic count, stromal overgrowth, and nature of their tumor borders.6 While grade of phyllodes is difficult to distinguish, distinguishing phyllodes from other fibroepithelial tumors can be difficult. Increased stromal cellularity is the distinguishing feature between a benign phyllodes tumor and fibroadenoma.6 In addition to histologic similarities, some limited evidence supports the development of phyllodes from fibroadenoma.6,7 Some advocate for assigning fibroadenoma and benign phyllodes in the pediatric population a similar category of disease, especially since most pediatric fibroepithelial tumors are biologically benign and rarely recur.3 This case highlights the relationship, and possible continuum, between fibroadenoma and phyllodes tumors given the diagnoses of fibroadenoma, fibroepithelial lesion, and phyllodes tumor prescribed by various pathologists.
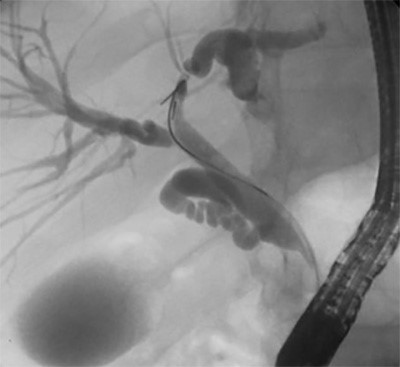
Cyclosporine, in distinction to other immunosuppressive agents, has been implicated in the development of fibroadenoma in post-renal transplant patients. 8,9,10,11,12 In patients taking cyclosporine, benign breast disease is increased compared to the general population.13,14 Cyclosporine associated fibroadenoma after renal transplant was first reported in 1980 and is well documented.8,9,10,11,12,15 This association seems to be unique to renal transplant patients as increased risk of fibroadenoma has not been observed after thoracic transplantation with short term immunosuppression.16 While fibroadenoma are the most common breast tumors associated with cyclosporine, fibrocystic lesions, intraductal papillomatosis, and invasive cancer has also been described.14 This case highlights the association between cyclosporine and fibroadenoma, and to our knowledge, is the first reported case of phyllodes tumor after renal transplant, and the first cyclosporine associated perineal phyllodes tumor.
In contrast to fibroadenoma, which are common among the general population, phyllodes tumors comprise less than 1% of breast tumors.17 Isolated reports of phyllodes tumors after liver transplantation and thoracic organ transplantation exist.16,18 As mammary glands are found in the vulva, case reports also describe phyllodes lesions in the anogenital region.19 However, none describe an association with cyclosporine.
While surgical resection is recommended for phyllodes tumors, intervention for fibroadenoma depends on risk factors including age greater than thirty-five, mass immobility, or size greater than 2.5 centimeters.17,20 For cyclosporine associated tumors, discontinuation of cyclosporine is also necessary. The pathophysiology of cyclosporine induced tumor development remains unclear and may include effects on fibroblasts, the hypothalamopituitary axis, or growth factors.21,22,23,24 After transitioning to an alternative immunosuppressive agent, reports show that 38% fibroadenoma resolved and the others decreased in size or remained stable.25 As such, cessation of cyclosporine is necessary to promote regression. Continued exposure to cyclosporine promoted tumor growth in this patient. Clinicians must consider inciting agents as possible etiology for continued recurrent pathology in adolescent patients.
Conclusion
We highlight the rare case of cyclosporine associated phyllodes tumors and fibroadenoma after renal transplantation. Breast lesions in the pediatric population are exceedingly rare and the etiology of which must be further explored to prevent unnecessary surgeries. While surgery is considered standard of care for phyllodes tumors and certain fibroadenoma, cyclosporine associated tumors also require transition to an alternative immunosuppressive agent to prevent further recurrence.
Lessons Learned
Fibroadenoma are common breast tumors in adults and, when present, in adolescents. Fibroepithelial lesions include both fibroadenoma and phyllodes tumors and may be difficult to distinguish from one another and may fall along a continuum rather than as separate entities. Consideration regarding the etiology of abnormal breast lesions in a pediatric patient must include immunosuppressive medications. Discontinuation of the drug and transition to an alternative immunosuppressive agent is a necessary component of tumor recurrence prevention.
Acknowledgments
We would like to thank the Pathology Department at Kapi'olani Medical Center for Women and Children for their assistance obtaining the pathology slides.
Authors
Authors
Ashley D. Marumoto, MD
University of Hawaii, John A. Burns School of Medicine
Department of Surgery
Honolulu, HI 96813
Sidney M. Johnson, MD
University of Hawaii, John A. Burns School of Medicine
Department of Surgery
Honolulu, HI 96813
and
Kapi'olani Medical Center for Women and Children
Department of Pediatric Surgery
Honolulu, HI 96826
Correspondence
Dr. Sidney Johnson
Department of Pediatric Surgery
Kapi'olani Medical Center for Women and Children
1319 Punahou Street, #600
Honolulu, HI, 96826
Phone: 808-983-6210
E-mail: sidney.johnson@kapiolani.org
Disclosures
The authors have no conflicts of interest or financial disclosures to declare.
References
- Lee EJ, Chang Y-W, Oh JH, Hwang J, Hong SS, Kim H-J. Breast Lesions in Children and Adolescents: Diagnosis and Management. Korean J Radiol. 2018 Oct;19(5):978–91.
- Sanders LM, Sharma P, El Madany M, King AB, Goodman KS, Sanders AE. Clinical breast concerns in low-risk pediatric patients: practice review with proposed recommendations. Pediatr Radiol. 2018;48(2):186–95.
- Tay TKY, Chang KTE, Thike AA, Tan PH. Paediatric fibroepithelial lesions revisited: pathological insights. J Clin Pathol. 2015 Aug 1;68(8):633–41.
- Lawton TJ, Acs G, Argani P, Farshid G, Gilcrease M, Goldstein N, et al. Interobserver variability by pathologists in the distinction between cellular fibroadenomas and phyllodes tumors. Int J Surg Pathol. 2014 Dec;22(8):695–8.
- Yang X, Kandil D, Cosar EF, Khan A. Fibroepithelial Tumors of the Breast: Pathologic and Immunohistochemical Features and Molecular Mechanisms. Arch Pathol Lab Med. 2013 Dec 30;138(1):25–36.
- Tan BY, Acs G, Apple SK, Badve S, Bleiweiss IJ, Brogi E, et al. Phyllodes tumours of the breast: a consensus review. Histopathology. 2016 Jan;68(1):5–21.
- Pareja F, Geyer FC, Kumar R, Selenica P, Piscuoglio S, Ng CKY, et al. Phyllodes tumors with and without fibroadenoma-like areas display distinct genomic features and may evolve through distinct pathways. NPJ Breast Cancer. 2017;3:40.
- Alkhunaizi AM, Ismail A, Yousif BM. Breast fibroadenomas in renal transplant recipients. Transplant Proc. 2004 Aug;36(6):1839–40.
- Rolles K, Calne RY. Two cases of benign lumps after treatment with cyclosporin A. Lancet Lond Engl. 1980 Oct 11;2(8198):795.
- Baildam AD, Higgins RM, Hurley E, Furlong A, Walls J, Venning MC, et al. Cyclosporin A and multiple fibroadenomas of the breast. Br J Surg. 1996 Dec;83(12):1755–7.
- Son EJ, Oh KK, Kim EK, Cho N, Lee JD, Kim SH, et al. Characteristic imaging features of breast fibroadenomas in women given cyclosporin A after renal transplantation. J Clin Ultrasound JCU. 2004 Feb;32(2):69–77.
- Binokay F, Balal M, Demir E, Paydas S, Soyupak S, Sertdemir Y, et al. Risk of developing fibroadenoma with the use of cyclosporine A in renal transplant recipients. Ren Fail. 2005;27(6):721–5.
- Stewart T, Tsai SC, Grayson H, Henderson R, Opelz G. Incidence of de-novo breast cancer in women chronically immunosuppressed after organ transplantation. Lancet Lond Engl. 1995 Sep 23;346(8978):796–8.
- Sangthawan P, Fox J, Atkins RC, Kerr PG. Increased incidence of benign breast disease in female renal transplant patients receiving cyclosporin. ANZ J Surg. 2002 Mar;72(3):222–5.
- Kollias J, Gill PG, Leong AS, Clarkson AR. Gynaecomastia presenting as fibroadenomatoid tumours of the breast in a renal transplant recipient associated with cyclosporin treatment. ANZ J Surg. 1998 Sep;68(9):679–81.
- Campbell A, Moazami N, Ditkoff BA, Kurtz E, Estabrook A, Schnabel F. Short-term outcome of chronic immunosuppression on the development of breast lesions in premenopausal heart and lung transplant patients. J Surg Res. 1998 Jul 15;78(1):27–30.
- Spitaleri G, Toesca A, Botteri E, Bottiglieri L, Rotmensz N, Boselli S, et al. Breast phyllodes tumor: a review of literature and a single center retrospective series analysis. Crit Rev Oncol Hematol. 2013 Nov;88(2):427–36.
- Cheng F, Qin J, Yu M, Zhang F, Li X, Sun B, et al. De novo phyllodes tumor in an adolescent female after liver transplantation. Pediatr Transplant. 2011 Feb;15(1):E12-14.
- Denlinger LN, Lokhandwala PM, Abendroth CS. Benign Phyllodes Tumor of the Vulva: A Case Report and Literature Review. Rare Tumors. 2015 Dec 29;7(4):6010.
- Hubbard JL, Cagle K, Davis JW, Kaups KL, Kodama M. Criteria for excision of suspected fibroadenomas of the breast. Am J Surg. 2015 Feb;209(2):297–301.
- Rajfer J, Sikka SC, Lemmi C, Koyle MA. Cyclosporine inhibits testosterone biosynthesis in the rat testis. Endocrinology. 1987 Aug;121(2):586–9.
- Campistol JM, Iñigo P, Larios S, Bescos M, Oppenheimer F. Role of transforming growth factor-beta1 in the progression of chronic allograft nephropathy. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc—Eur Ren Assoc. 2001;16 Suppl 1:114–6.
- Tyldesley WR, Rotter E. Gingival hyperplasia induced by cyclosporin-A. Br Dent J. 1984 Nov 10;157(9):305–9.
- Schincaglia GP, Forniti F, Cavallini R, Piva R, Calura G, del Senno L. Cyclosporin-A increases type I procollagen production and mRNA level in human gingival fibroblasts in vitro. J Oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol. 1992 Apr;21(4):181–5.
- Iaria G, Pisani F, De Luca L, Sforza D, Manuelli M, Perrone L, et al. Prospective study of switch from cyclosporine to tacrolimus for fibroadenomas of the breast in kidney transplantation. Transplant Proc. 2010 May;42(4):1169–70.