Abstract
Background
Ileocaval venous obstruction in kidney transplant recipients may preclude a conventional external iliac venous anastomosis if adequate allograft venous outflow cannot be achieved. We share the case of a 69-year-old male with a history of inferior vena cava (IVC) ligation who presented for kidney transplantation. A unique surgical approach was utilized for venous drainage of an iliac fossa deceased-donor allograft.
Summary
Our patient presented for a deceased-donor renal transplant. He had a history of deep vein thrombosis (DVT) requiring remote infrarenal IVC ligation after developing intraabdominal bleeding while on anticoagulation. After inspection of the patient’s computed tomography (CT) imaging and the deceased-donor right kidney, which had been procured with a substantial length of proximal IVC, he was deemed a candidate for iliac fossa allograft implantation using an inverted donor IVC conduit. The donor renal vein was divided from the donor IVC, then rotated 180º. The donor renal vein was re-implanted at its original orifice, creating a conduit from the renal hilum running superiorly. An end-to-side anastomosis between the inverted donor IVC and recipient IVC was created above the IVC obstruction. He experienced immediate and sustained allograft function at his latest follow-up three months post transplantation.
Conclusion
Iliac vein and IVC anomalies represent a surgical challenge for renal transplantation. We present a case where an inverted donor IVC conduit was created to bypass an infrarenal IVC obstruction, resulting in successful iliac fossa allograft implantation. This case highlights how preoperative planning, procedural creativity, and knowledge regarding alternative venous drainage options and implantation sites for renal allografts can assist in identifying solutions to these technical challenges.
Key Words
kidney transplantation; surgical technique; ileocaval obstruction
Abbreviations
COPD: chronic obstructive pulmonary disorder
DOAC: direct-acting oral anticoagulant
DVT: deep vein thrombosis
GSV: greater saphenous vein
IVC: inferior vena cava
PE: pulmonary embolism
Case Description
Ileocaval venous obstruction can be caused by a variety of etiologies, including congenital atresia, thrombosis, or iatrogenic. When present in renal transplant recipients, these anomalies may preclude a conventional external iliac venous anastomosis, as a low-pressure venous outflow from the allograft is required to minimize the risk of graft failure. The patient should therefore be evaluated for an alternative site of venous drainage. The anatomical characteristics of the procured organ may also influence the surgical approach. We report a unique case of surgical management of a kidney transplant recipient with an inferior vena cava (IVC) obstruction.
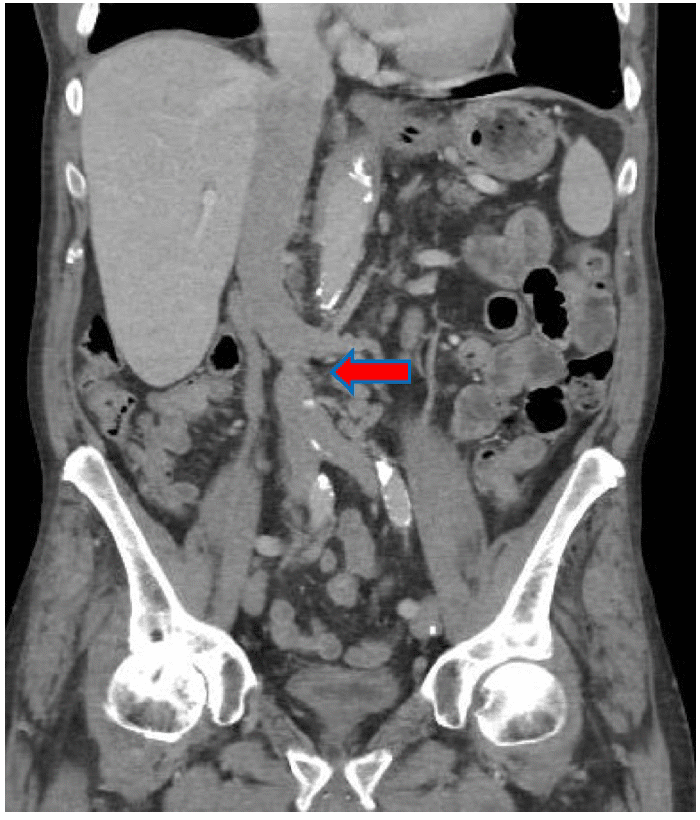
The patient is a 69-year-old male with a history of severe chronic obstructive pulmonary disorder (COPD) requiring bilateral lung transplants and end-stage renal disease secondary to resulting calcineurin toxicity, who presented to our institution for deceased-donor kidney transplantation. He also had a history of deep vein thrombosis and pulmonary embolism (DVT/PE) requiring remote infrarenal IVC ligation to prevent thrombosis propagation after developing intraabdominal bleeding while on anticoagulation. A computed tomography (CT) scan of the abdomen and pelvis was obtained on his arrival at our facility to delineate his abdominal venous outflow better and assist with surgical planning (Figure 1).
Figure 1. Location of Infrarenal IVC Ligation (arrow). Published with Permission
The right-sided deceased donor kidney was then inspected. The donor renal vein had been procured along with 2 cm proximal and 8 cm distal donor IVC. The patient was taken to the operating room for a planned renal transplant in the right iliac fossa, using recipient IVC just proximal to his obstruction as the site for venous drainage of the allograft. An inverted donor IVC conduit was created to maximize the proximity of the allograft to the right iliac artery and bladder. The donor renal vein was divided from the donor IVC, which was then rotated 180º. The donor renal vein was re-implanted at its original orifice, now at the inferior aspect of the IVC, creating a conduit from the renal hilum running superiorly. The inferior IVC cuff was then oversewn. A right lower quadrant curvilinear incision and a right retroperitoneal dissection were performed (Figure 2).
Figure 2. Intraoperative Photo. Published with Permission
An end-to-side anastomosis between the inverted donor IVC and recipient IVC was created above the obstruction and below the native renal veins, and an end-to-side anastomosis between the donor renal artery and recipient external iliac artery was created (Figure 3). A Lich ureterocystostomy was then performed.
Figure 3. Intraoperative Photo. Published with Permission
There were no surgical complications, and the patient experienced immediate allograft function. He was discharged on postoperative day 7. Graft function has remained excellent at his latest follow-up three months post-transplantation.
Discussion
Ileocaval venous anomalies in kidney transplant recipients present a technical challenge to renal transplantation. Venous anomalies may be identified by patient history, physical exam, preoperative imaging, or incidentally intraoperatively. They can be due to various etiologies, including thrombosis, congenital agenesis, extrinsic compression, or intrinsic stenosis due to intraluminal devices. An ileocaval anomaly impeding venous outflow is not an absolute contraindication to conventional external iliac venous anastomosis; there are case reports of successful renal transplantation when patients are maintained on lifelong anticoagulation, and collateral drainage was deemed adequate on venography.1,2 However, high-pressure venous outflow can lead to acute renal vein thrombosis, graft failure, delayed thrombosis,3 chronic graft dysfunction,4 and or abdominal wall phlebitis.5 Therefore, an iliac vein or IVC anomaly in a potential kidney transplant recipient should prompt evaluation of ileocaval venous outflow and consider alternative venous drainage options and allograft implantation sites, taking into account both patient and allograft anatomy.
Successful renal transplantation using nontraditional venous drainage sites has been widely reported and can be broadly categorized into systemic or portal venous anastomoses. Systemic options amenable to iliac fossa graft placement include the IVC,1,4,6-10 large collateral vein,10-12 or gonadal vein.13-15 An orthotopic placement using the native renal vein,4,16 is another systemic option, though a native nephrectomy is also often required to create space for the graft. Portal venous drainage options require intraabdominal graft placement and are, therefore, at a greater risk of vascular torsion compared to retroperitoneal graft placement. Portal options include the splenic vein,7,17-20 IMV,21,22 SMV,16,23,24 portal vein,16,25,26 and hepatic vein.27
Our patient’s preoperative imaging demonstrated a patent portion of his infrarenal IVC, which could be easily accessed through an elongated paramedian incision allowing for iliac fossa placement, which was preferred due to its proximity to the iliac artery and bladder. However, elongation of the donor renal vein was required to reach the patent IVC. There are two case reports where an extension of the donor renal vein was used to reach its destination; one case used a donor iliac vein interposition graft to bridge the donor renal vein to the recipient portal vein,25 while the other involved procurement of the ovarian vein and greater saphenous vein (GSV) along with the kidney from a living donor.6 In the latter case, the GSV was ultimately used to bridge the donor renal vein to the infrahepatic IVC. Our case demonstrates that the donor IVC procured with the deceased-donor allograft is another valuable option for renal vein elongation and may be inverted to bridge the donor renal vein and the recipient infrarenal IVC.
Conclusion
Iliac vein and IVC anomalies in kidney transplant recipients preclude a conventional external iliac venous anastomosis if there is potential for allograft venous outflow hypertension. These anomalies should prompt consideration of alternative systemic or portal venous drainage options, which may require orthotopic or intraabdominal graft placement. Both patient and allograft anatomy can influence the surgical approach. We report a case of a successful kidney transplant in a patient with an infrarenal IVC obstruction, where the patient and allograft anatomy allowed for an iliac fossa placement of a graft using an inverted donor IVC conduit to bypass his IVC obstruction.
Lessons Learned
Ileocaval venous anomalies in kidney transplant recipients should prompt consideration of unconventional venous drainage options. Both patient and allograft anatomy inform surgical decision-making. An infrarenal IVC obstruction can be successfully bypassed using an inverted donor IVC conduit for venous drainage of an iliac fossa deceased-donor allograft.
Authors
Sweet ALa; Scott DLa,b; Connelly CRa,b
Author Affiliations
- Department of Surgery, Oregon Health & Science University, Portland, OR 97239
- Department of Surgery, VA Portland Health Care System, Portland, OR 97239
Corresponding Author
Ashley L. Sweet, MD, MBE
3181 SW Sam Jackson Park Road
Mail Code L223
Portland, OR 97239
Email: sweetas@ohsu.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: May 5, 2021
Accepted: July 5, 2021
References
- Shenoy M, Pararajasingam R, Wright NB, et al. Successful renal transplantation in children in the presence of thrombosis of the inferior vena cava. Pediatr Nephrol. 2008;23(12):2261-2265. doi:10.1007/s00467-007-0736-3
- ElMalik EM, Fernando ON. Renal transplantation in patients with complete obstruction of the inferior vena cava. Urology. 1999;53(6):1228. doi:10.1016/s0090-4295(98)00522-6
- Thiessen L, MacDonell S, Wall C, Jacob P, Shoker A, Moser MAJ. Transplant renal vein thrombosis in a recipient with aberrant venous anatomy. CEN Case Rep. 2018;7(2):264-267. doi:10.1007/s13730-018-0340-3
- Martinez-Urrutia MJ, Pereira PL, Ramirez LA, et al. Renal transplant in children with previous inferior vena cava thrombosis. Pediatr Transplant. 2007;11(4):419-421. doi:10.1111/j.1399-3046.2007.00680.x
- Janssen S, van Donselaar-van der Pant KA, van der Weerd NC, et al. Abdominal wall phlebitis due to Prevotella bivia following renal transplantation in a patient with an occluded inferior vena cava. Infection. 2013;41(1):271-274. doi:10.1007/s15010-012-0335-5
- Muramatsu M, Shishido S, Takahashi Y, et al. Successful third renal transplantation in a child with an occluded inferior vena cava: A novel technique to use the venous interposition between the transplant renal vein and the infrahepatic inferior vena cava. Int J Urol. 2017;24(5):396-398. doi:10.1111/iju.13322
- Gil-Vernet JM, Gil-Vernet A, Caralps A, et al. Orthotopic renal transplant and results in 139 consecutive cases. J Urol. 1989;142(2 Pt 1):248-252. doi:10.1016/s0022-5347(17)38721-9
- Pirenne J, Benedetti E, Kashtan CE, et al. Kidney transplantation in the absence of the infrarenal vena cava. Transplantation. 1995;59(12):1739-1742. doi:10.1097/00007890-199506270-00018
- Stevens RB, Yannam GR, Hill BC, Rigley TH, Penn DM, Skorupa JY. Successful urgent transplantation of an adult kidney into a child with inferior vena cava thrombosis. Am J Transplant. 2009;9(8):1953-1956. doi:10.1111/j.1600-6143.2009.02687.x
- Shishido S, Kawamura T, Hamasaki Y, et al. Successful Kidney Transplantation in Children With a Compromised Inferior Vena Cava. Transplant Direct. 2016;2(6):e82. Published 2016 May 23. doi:10.1097/TXD.0000000000000592
- Stippel DL, Bangard C, Schleimer K, Koerber F, Beckurts KT, Hoppe B. Successful renal transplantation in a child with thrombosis of the inferior vena cava and both iliac veins. Transplant Proc. 2006;38(3):688-690. doi:10.1016/j.transproceed.2006.01.068
- Lugo-Baruqui JA, Velásquez CA, Chen LJ, Ciancio G, Burke GW. Renal Transplantation in a Patient With Unsuspected Inferior Vena Cava Obliteration. Transplantation. 2016;100(10):2230-2233. doi:10.1097/TP.0000000000001039
- Wong VK, Baker R, Patel J, Menon K, Ahmad N. Renal transplantation to the ovarian vein: a case report. Am J Transplant. 2008;8(5):1064-1066. doi:10.1111/j.1600-6143.2008.02185.x
- Guo FF, Shao ZQ, Li HL, Wang GJ, Zhu WB. Successful use of the dilated right spermatic cord vein for renal transplantation in a patient with congenital hypoplasia of the inferior vena cava. Transplant Proc. 2011;43(10):4002-4004. doi:10.1016/j.transproceed.2011.09.077
- Tao R, Shapiro R. Successful adult-to-child renal transplantation utilizing the ovarian vein in children with inferior vena cava/iliac vein thrombosis. Pediatr Transplant. 2010;14(6):E70-E74. doi:10.1111/j.1399-3046.2009.01132.x
- Lonze BE, Dagher NN, Alachkar N, Jackson AM, Montgomery RA. Nontraditional sites for vascular anastomoses to enable kidney transplantation in patients with major systemic venous thromboses. Clin Transplant. 2017;31(12):10.1111/ctr.13127. doi:10.1111/ctr.13127
- Rizzello A, Smyth O, Patel N, Reddy S, Sinha S, Vaidya A. Successful splenic venous drainage for kidney transplant in case of inferior vena cava thrombosis. Transplantation. 2011;92(10):e59-e60. doi:10.1097/TP.0b013e3182352d86
- Kumar S, Rathore Y, Guleria S, Bansal VK. Renal transplantation in a child with thrombosed inferior vena cava. Saudi J Kidney Dis Transpl. 2014;25(2):367-369. doi:10.4103/1319-2442.128546
- Marinov M, Di Domenico S, Mastrodomenico P, et al. Use of the splenic vessels for an ABO incompatible renal transplant in a patient with thrombosis of the vena cava. Am J Transplant. 2005;5(9):2336-2337. doi:10.1111/j.1600-6143.2005.00986.x
- Shapira Z, Yussim A, Savir A, et al. The use of the portal system for the transplantation of a neonate kidney graft in a child with Wilms’ tumor. J Pediatr Surg. 1985;20(5):549-551. doi:10.1016/s0022-3468(85)80487-5
- Rosenthal JT, Loo RK. Portal venous drainage for cadaveric renal transplantation. J Urol. 1990;144(4):969-971. doi:10.1016/s0022-5347(17)39635-0
- Patel P, Krishnamurthi V. Successful use of the inferior mesenteric vein for renal transplantation. Am J Transplant. 2003;3(8):1040-1042. doi:10.1034/j.1600-6143.2003.00177.x
- Aguirrezabalaga J, Novas S, Veiga F, et al. Renal transplantation with venous drainage through the superior mesenteric vein in cases of thrombosis of the inferior vena cava. Transplantation. 2002;74(3):413-415. doi:10.1097/00007890-200208150-00022
- Lonze BE, Dagher NN, Simpkins CE, et al. Eculizumab, bortezomib and kidney paired donation facilitate transplantation of a highly sensitized patient without vascular access. Am J Transplant. 2010;10(9):2154-2160. doi:10.1111/j.1600-6143.2010.03191.x
- Reinhardt R, Treckmann J, Radünz S, et al. Kidney transplantation in a patient with congenital vena cava and right vena iliaca communis hypoplasia. Transpl Int. 2010;23(9):e59-e61. doi:10.1111/j.1432-2277.2010.01129.x
- Millan M, Caicedo LA, Villegas JI, et al. Case report of cadaveric kidney transplantation with renal-portal venous drainage: A feasible way for a venous drainage in a complex generalized thrombosed vessels setting. Int J Surg Case Rep. 2016;28:192-195. doi:10.1016/j.ijscr.2016.09.047
- Verghese P, Minja E, Kirchner V, Chavers B, Matas A, Chinnakotla S. Successful Renal Transplantation in Small Children With a Completely Thrombosed Inferior Vena Cava. Am J Transplant. 2017;17(6):1670-1673. doi:10.1111/ajt.14213