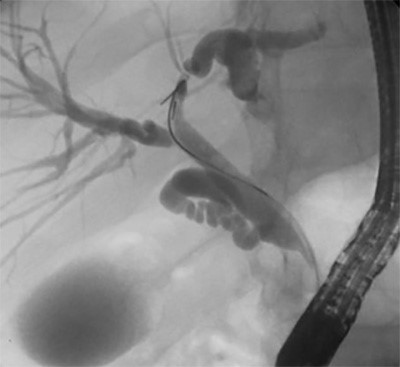
Figure 2. A laparoscopic image showing the tubularized stomach (an intraperitoneal sling) connecting to the anterior abdominal wall. Dilated loops of small bowel are visible in the background. A: gastric sling, B: dilated proximal small intestine, C: distal collapsed bowel, and D: terminal ileum
Once this attachment was dissected off of the anterior abdominal wall with a laparoscopic staple, the small intestine returned to its normal anatomic position and began to decompress. The remains of tubular structure originating from the gastrostomy site were then sutured to the remnant stomach with intracorporeal sutures in order to prevent re-attachment and possible recurrence of volvulus. The closures of the Petersen's space defect and small bowel mesenteric defect were intact. The patient was discharged on the first postoperative day and has experienced no further symptoms.
Discussion
In patients who have had a previous laparoscopic Roux-en-Y gastric bypass (LRYGBP) surgery, internal hernia is the most common cause of small bowel obstruction (SBO); it is also the most commonly missed SBO etiology on CT scan.4 On a review of 1,282 small bowel follow-throughs after a LRYGBP, an internal hernia was found in 20 (1.6 percent) patients.5 An internal hernia is caused by projection of bowel through a congenital or created foramen in the abdominal cavity. Other reported causes of SBO in post-LRYGBP patients include adhesions, ventral hernia, postoperative ileus and jejunojejunal anastomotic strictures, listed in order of descending prevalence. Notably, these etiologies may have very similar clinical presentations and diagnostic clues can include timing of presentation and imaging findings. Based on this patient's presentation and the common complications associated with her past surgical history, an internal hernia was considered the most likely cause of her symptoms.
Small bowel volvulus (SBV) is another rare cause of SBO that was in the differential. Volvulus entails twisting of the small bowel around its mesenteric axis. In adults, it accounts for 1.7 to 6.2 percent of SBOs1 and is typically secondary to adhesive bands, tumors or malrotation.2 Mortality is 9.3 percent, with higher mortality appreciated among patients with a history of abdominal surgery.3 It presents emergently in 89.2 percent of cases and is resolved operatively in 65.21 percent of cases.<2 The presentation is most commonly that of acute abdomen (abdominal pain, nausea, vomiting), but can be variable and nonspecific.6 In the case of intermittent volvulus, the presentation can be vague, making these cases difficult to diagnose. The preferred detection modality for SBV detection is abdominal CT scan with contrast with an accuracy of 83 percent.3 In cases of intermittent volvulus, it may not be possible to identify the anatomic abnormality via imaging modalities. Thus, diagnostic laparoscopy remains the most effective way to identify and treat the problem in these patients. Due to this patient's presentation of intermittently severe obstructive symptoms and her history of disrupted normal gastrointestinal anatomy, SBV was also considered a possible cause of her symptoms. According to Cho et al., her surgical history made jejunojejunal anastomotic stenosis the most likely cause of her presentation.7
The cause of this patient's partial SBO symptoms, an intraperitoneal sling, has features of both a volvulus and of an internal hernia, yet does not conform to the definition of either. Like a volvulus, the vascular supply of the small intestine was compressed by twisting of the mesentery. However, unlike a volvulus, this twisting is not mesoaxial, but is instead due to twisting around a noncontiguous structure. Similarly, like an internal hernia, the small intestine can be seen as passing through a defect that compresses both vasculature and the intestinal lumen. Unlike an internal hernia defect, whose boundaries are easily defined, the boundaries of a sling-related "internal hernia" are arbitrary. In this case, for example, we could arbitrarily define the hernia orifice as the sling medially, the left anterior abdominal wall anteriorly, and the stomach and transverse colon posteriorly. Just as validly, we could define the defect as the sling inferiorly, the anterior abdominal wall and diaphragm anteriorly, and the stomach posteriorly. It is the arbitrary nature of the defect boundaries that separates the intraperitoneal sling from the large orifice hernia, yet both may have a similar clinical presentation.
In our patient, a tubularized structure that had formed from her prior gastrostomy site was discovered as the culprit. Laparoscopic gastrostomy tube placement is a common procedure with a high success rate (96 percent). However, it has a complication rate of 8 to 10 percent,8,9 which include skin pressure necrosis, extraluminal migration, wound infection, gastrointestinal bleeding, gastrocutaneous fistula, and failed placement. Cases of rotation of bowel loops around postsurgical or congenital adhesive bands and stoma are commonly reported in the literature.4 A case of an anterior gastropexy band giving rise to SBV has also been reported.10 However, the presence of a tubularized gastric structure, called here as an intraperitoneal sling, has not been previously reported. Furthermore, there have been no previous reports of gastrostomy tube site tubularization. The patient's symptoms did not suggest one of the common complications. The cause for the tubularization remains unknown, but possible contributing factors may include chronic inflammation, percutaneous endoscopic gastrostomy (PEG) manipulation, and excessive tension on the anterior stomach from the gastric tube and fixation sutures.
Conclusion
We present an unusual case of bowel obstruction resulting from a very commonly performed procedure (gastrostomy tube placement). The patient's symptoms and surgical history suggested an etiology of internal hernia or SBV. Exploratory laparoscopy revealed the presence of a previously unreported intraperitoneal sling and enabled curative treatment.
Lessons Learned
In this rare case of intermittent obstruction around a tubularized prior gastrostomy site in a patient with a history of Roux-en-Y gastric bypass, the presentation and history suggested internal hernia or SBV. However, curative diagnostic laparoscopy revealed that an intraperitoneal sling was responsible for her symptoms.
Authors
Kaylie Miller
School of Medicine, University of Maryland, Baltimore, MD
Syed Nabeel Zafar, MBBS MPH
Department of Surgery, University of Maryland, Baltimore MD
Mark Kligman, MD
Department of Surgery, University of Maryland, Baltimore MD
Correspondence Author
Dr. Mark Kligman
Assistant Professor
Director, Center for Weight Management & Wellness
University of Maryland Medical Center
Baltimore, MD 21201
Phone: 410-328-8940
Email: MKligman@som.umaryland.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Valsdottir E, Marks JH. Volvulus: small bowel and colon. Clin Colon Rectal Surg. May 2008;21(2):91–93.
- Coe TM, Chang DC, Sicklick JK. Small bowel volvulus in the adult populace of the United States: results from a population-based study. Am J of Surg. Aug 2015;210(2):201–210 e202.
- Ruiz-Tovar J, Morales V, Sanjuanbenito A, Lobo E, Martinez-Molina E. Volvulus of the small bowel in adults. Am Surg. Dec 2009;75(12):1179–1182.
- Gunabushanam G, Shankar S, Czerniach DR, Kelly JJ, Perugini RA. Small-bowel obstruction after laparoscopic Roux-en-Y gastric bypass surgery. J Comput Assist Tomogr. May-Jun 2009;33(3):369–375.
- Carucci LR, Turner MA, Shaylor SD. Internal hernia following Roux-en-Y gastric bypass surgery for morbid obesity: evaluation of radiographic findings at small-bowel examination. Radiology. Jun 2009;251(3):762–770.
- Roggo A, Ottinger LW. Acute small bowel volvulus in adults. A sporadic form of strangulating intestinal obstruction. Ann Surg. Aug 1992;216(2):135–141.
- Cho M, Carrodeguas L, Pinto D. Diagnosis and management of partial small bowel obstruction after laparoscopic antecolic antegastric Roux-en-Y gastric bypass for morbid obesity. J Am Coll Surg 2006;202 (2) 262–268
- Murayama KM, Johnson TJ, Thompson JS. Laparoscopic gastrostomy and jejunostomy are safe and effective for obtaining enteral access. Am J of Surg. Nov 1996;172(5):591–594; discussion 594–595.
- Peitgen K, von Ostau C, Walz MK. Laparoscopic gastrostomy: results of 121 patients over 7 years. Surg Laparosc Endosc Percutan Tech. Apr 2001;11(2):76–82.
- Khan ZAJ, Drye E, Pardeep S, Novell JR. Small Bowel Volvulus Resulting in Infarction due to an Anterior Gastropexy Band. JSLS. 2002;6(1):77–79.