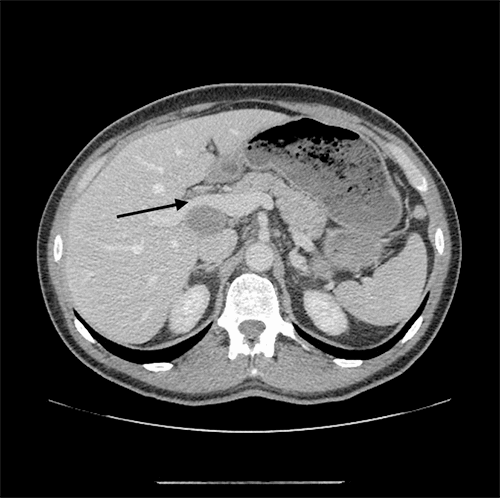
Figure 4: Patient’s gallbladder opened to reveal 10 x 5.5 x 4 cm mass
The case was reviewed at our multidisciplinary GI oncology tumor board, and the recommendation was to proceed with cisplatin and etoposide chemotherapy (CTx) followed by chemoradiation (CRTx). The patient tolerated his adjuvant treatment and following completion, the tumor board recommendation was to proceed with full surgical clearance of disease. A laparoscopic resection of extrahepatic bile ducts, resection of his type 1B choledochal cyst, partial hepatectomy of segments 4B and 5, portal lymphadenectomy, and reconstruction via a Roux-en-Y hepaticojejunostomy was performed. Intraoperatively, the patient was noted to have an extensive amount of scarring due to his prior surgery and chemoradiation; however, there was no evidence of metastatic disease. His bowel was also run intraoperatively to rule out primary small bowel NET. His station 8A lymph node was sent for frozen section, which was negative. His postoperative pathology demonstrated evidence of complete tumor death/fibrosis (no residual cancer); thus, the patient had a complete response to adjuvant CTx and CRTx. The patient tolerated the procedure well and was discharged home on postoperative day seven following an uneventful hospital course. Postoperative surveillance via MRI every three months has shown the patient to be disease-free; now 12 months postsurgery, future surveillance will be via MRI every via months.
Discussion
Primary gallbladder neuroendocrine tumors are a rare diagnosis,1 with only 278 cases described between 1975 and 2005 in the Surveillance, Epidemiology and End Results (SEER) program of the National Cancer Institute. GB-NETs represent less than one percent of all GEP-NETs and 0.5 percent of all gallbladder carcinomas and are an exceedingly unusual cause of gallbladder presentations.2,3,4 As a consequence, the natural history of such tumors are poorly understood, and recommendations for management and surveillance are variable across institutions. Primary adenocarcinomas of the gallbladder, conversely, are relatively far more frequent then GB-NETs and demonstrate an exceptionally aggressive phenotype. Though surgical resection provides the only possibility for cure, only 10 percent of patients present with resectable disease.5 All-stage, five-year survival remains dismal at less than five percent. Furthermore, the role of CTx and CRTx remains undefined, though combination platinum-based therapy has been most commonly utilized with some success.
GB-NETs pose a unique challenge to the clinician, as it is unknown whether they behave in a fashion similar to other GEP-NETs or if they more strongly resemble their epithelial counterpart. NETs are neoplasms originating from neuroendocrine cells (enterochromaffin cells) located throughout the body, typically within the lung and gastrointestinal tract.3 The origin of GB-NETs, however, is poorly understood, since the normal gallbladder mucosa is typically devoid of neuroendocrine cells. It is currently postulated that neuroendocrine cells may arise in the gallbladder secondary to chronic inflammation caused by gallstones, helicobacter pylori, or congenital anomalies, such as anomalous union of the pancreaticobiliary duct or choledochal cysts as seen in our patient.6,7
The 2010 World Health Organization (WHO) classification of NETs describes four general categories based primarily on mitotic count and Ki-67 proliferative index: well differentiated NET or Grade 1 tumor (Ki-67 <three percent); intermediate differentiated NET or Grade 2 tumor (Ki-67 <3–20 percent); poorly differentiated neuroendocrine carcinoma (NEC) or Grade 3 tumor (Ki-67 >20 percent); and mixed adenoneuroendocrine carcinoma (MANEC).8 Poorly differentiated NECs have a high propensity for invasive growth, early lymph node metastases, as well as distant metastases and generally have a poor prognosis.7,9-13
NECs are further classified into the more common small-cell type and the less common large-cell type, which behave similar to lung NECs. Though initially considered to behave like small-cell NECs, more recent reports have demonstrated improved prognosis in large-cell variants.14 The role of surgery in NEC remains undefined, though may provide an avenue for cure in patients with locoregional disease.15 Similarly, the role and benefit of CTx and CRTx in the neoadjuvant/adjuvant setting is unclear, though both have been employed in patients with locoregional disease. Shimono et al discussed a case of gallbladder NEC successfully treated via multimodal therapies inclusive of CT-based three-dimensional radiation therapy administered preoperatively.16 Further, Chen et al discussed three cases of GB-NEC treated with postoperative CRTx versus surgery alone with nonsignificant increases in median survival times for those receiving multimodal treatment.17 CTx is generally platinum-based combined with etoposide, and tumors typically demonstrate responsiveness in patients with Ki-67 >55 percent.18 Our case report adds to the existing literature of GB-NETs and highlights the possibility of such tumors presenting as biliary colic. Though this is an exceedingly rare cause of biliary colic, awareness of its existence is important for the clinician when considering atypical etiologies of gallbladder pathologies that may prompt earlier involvement of a hepatobiliary surgeon. The current case report also emphasizes the absolute need for a multidisciplinary approach and the involvement of both a medical and radiation oncologist. We have demonstrated that combination treatment with surgery, CTx, and CRTx is effective, and though the tumor demonstrated a Ki-67 >55 percent, complete disease remission is possible.
Conclusion
While the patient has remained disease-free for 12 months following surgical resection, continued surveillance is required to determine if these interventions will yield a disease-free/overall survival comparable to the broader category of GEP-NETs.
Lessons Learned
GB-NETs are a rare subtype of gallbladder cancers which may have a possibility of cure when managed in a multidisciplinary setting. The pathophysiology of the disease is unknown; thus longer follow-up may help clarify its natural history in patients treated with combined modalities.
Authors
Christina N. Weed, MD, MPH
Virginia Mason Medical Center
Division of General, Thoracic and Vascular Surgery
Seattle, WA
Zaheer S. Kanji MD, MSc, FRCSC
Virginia Mason Medical Center
Division of General, Thoracic and Vascular Surgery
Seattle, WA
Adnan A. Alseidi MD, EdM, FACS
Virginia Mason Medical Center
Division of General, Thoracic and Vascular Surgery
Seattle, WA
Correspondence Author
Adnan A. Alseidi MD, EdM, FACS
Virginia Mason Medical Center
Division of General, Thoracic and Vascular Surgery
6th Floor Buck Pavilion, C6-GS
1100 9th Avenue
Seattle, WA 98101
Adnan.Alseidi@virginiamason.org
Disclosure Statement
Drs. Weed, Kanji, and Alseidi have no conflicts of interest or financial disclosures to report.
References
- Joel W. Karzinoid der Gallenblasse. Zentral-bl Allg Pathol. 1929;46:1–4.
- The US National Cancer Institute. Surveillance Epidemiology and End Results (SEER) data base, 1973-2005. http://seer.cancer.gov/. 2008.
- Yao JC, Hassan M, Phan A, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26(18):3063-72.
- Gupta A, Ahmed P, Durgapal P et al. Neuroendocrine Carcinoma of the Gallbladder: A rare presentation with review of the literature. Gulf J Oncolog. 2017 May; 1(24): 51-54
- Zhu AX, Hong TS, Hezel AF, Kooby DA. Current Management of Gallbladder Carcinoma. Oncologist. 2010;15(2):168-181. doi:10.1634/theoncologist.2009-0302.
- Liu W, Wang L, He X, Feng C, Chang X, Lu Z. Mixed large cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder: a case report and brief review of the literature. World J Surg Oncol. 2015;13:114. doi:10.1186/s12957-015-0533-6.
- Jun SR, Lee JM, Han JK, et al. High-grade neuroendocrine carcinomas of the gallbladder and bile duct: report of four cases with pathological correlation. J Comput Assist Tomogr. 2006;30:604–609
- Rindi G. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon, France: The International Agency for Research on Cancer; 2010. pp. 13–4.
- Buscemi S, Orlando E, Damiano G, et al. "Pure" large cell neuroendocrine carcinoma of the gallbladder. Report of a case and review of the literature. Int J Surg. 2016;28:S128-32. doi:10.1016/j.ijsu.2015.12.045.
- Furrukh M, Qureshi A, Saparamadu A, Kumar S. Malignant neuroendocrine tumour of the gallbladder with elevated carcinoembryonic antigen: case report and literature review. BMJ Case Rep. 2013;2013:bcr2013008778. doi:10.1136/bcr-2013-008778.
- 11Kamboj M, Gandhi JS, Gupta G. Neuroendocrine Carcinoma of the Gallbladder: A Series of 19 Cases and Review of the Literature. J Gastrointest Cancer. 2015;46(4):356-364. doi: 10.1007/s12029-015-9745-9.
- Chen H, Shen YY, Ni XZ. Two cases of neuroendocrine carcinoma of the gallbladder. World J Gastroenterol. 2014;20(33):11916-11920. doi:10.3748/wjg.v20.i33.11916.
- Carrera C, Kunk P, Rahma O. Small Cell Carcinoma of the Gallbladder: Case Report and Comprehensive Analysis of Published Cases. J Oncol. 2015;2015:304909. doi:10.1155/2015/304909.
- Korse CM, Taal BG et al. Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer. 2013 May; 49 (8): 1975-83.
- 15Haugvik, SP, Janson ET, Osterlund P et al. Surgical Treatment as a Principle for Patients with High Grade Pancreatic Neuroendocrine Carcinoma: A Nordic Multicenter Comparative Study. Ann Surg Oncol. 2016 May; 23 (5): 1721-8.
- Shimono C, Suwa K, Sato M, et al. Large cell neuroendocrine carcinoma of the gallbladder: Long survival achieved by multimodal treatment. Int J Clin Oncol. 2009;14(4):351-5. doi: http://dx.doi.org/10.1007/s10147-008-0843-6.
- Chen C, Wang L, Liu X, Zhang G, Zhao Y, Geng Z. Gallbladder neuroendocrine carcinoma: report of 10 cases and comparison of clinicopathologic features with gallbladder adenocarcinoma. Int J Clin Exp Pathol. 2015;8(7):8218-8226.
- Sorbye H, Welin S, Langer SW et al. Predictive and Prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC Study. Ann Oncol. 2013 Jan; 24(1): 152-60.