The patient was admitted to the surgical service to treat cellulitis of the previous incision and drainage site. She was given Piperacillin-Tazobactam and underwent local wound care to her previous cholecystostomy tube site with gallbladder herniation. Operative management of her gallbladder herniation was not pursued as the patient remained a poor surgical candidate. The patient's symptoms improved with antibiotic treatment, and she was sent home with nursing services for wound care as well as a complete course of oral antibiotics.
Case Discussion
Herniation of the gallbladder is a rare complication of gallstone disease, and the few published case reports are mostly associated with incisional, parastomal, ventral, and epigastric hernias.1‒10 This is the first report in the literature of spontaneous extrusion of gallbladder through a cholecystocutaneous fistula after removing a percutaneous cholecystostomy tube. There are short-term and long-term complications associated with percutaneous cholecystostomy tube placement. Immediate complications of PCT include biliary peritonitis, sepsis, tube blockage, pain, and tube dislodgement. These complications are becoming less frequent as technique and imaging modality evolve.11‒14 Cholecystostomy tube placement is a procedure with high technical success and acceptably low complication and mortality rates.15,16 Cholecystitis recurrence and hospital readmission rates following PCT have been reported to be as high as 41 percent.17 While PCT is a viable option for high-risk patients unable to tolerate cholecystectomy, it is not a definitive solution for acute cholecystitis as most patients should undergo an interval cholecystectomy.
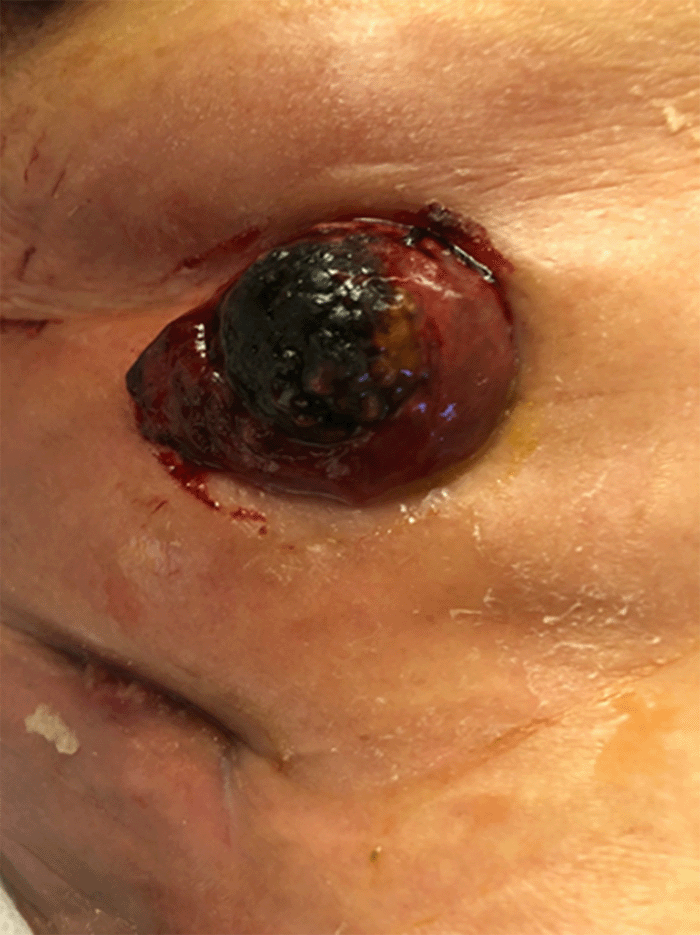
The majority of patients do well following removal of the drain with the eventual closure of the drain site by secondary intention. However, if the patient continues to have large gallstones within the gallbladder that are not draining through the cystic duct or cholecystostomy tube, this can be problematic. Since our patient did not proceed with an interval cholecystectomy after removal of PCT, she remained at risk for developing recurrent cholecystitis. Her imaging showed she had persistent cholelithiasis, and although cholecystocutaneous fistulas occur in acalculous cholecystitis and gallbladder carcinoma, gallstones remain the most common risk factor for developing a fistula.17 Given the large size of the patient's gallstone, the cystic duct was likely occluded, leading to increased pressure in the gallbladder causing mural necrosis and perforation due to compromised blood flow and impairs lymphatic drainage.17,18 This chronic inflammation most likely prevented our patient's cholecystocutaneous fistula from healing. Further, her poor nutritional status may have also contributed to the development of gallbladder wall herniation. Although no nutrition markers were obtained during her initial presentation, her albumin and prealbumin levels were low at 3.3 gm/dl and 10.8 mg/dl, respectively, a year prior.
Conclusion
In summary, we present a rare case of gallbladder herniation and cholecystocutaneous fistula formation after percutaneous cholecystostomy tube placement. To our knowledge, this is the first reported case of gallbladder herniation and fistulization after PCT drain removal. This anomaly was specifically managed non-operatively with gallstone dislodgement, local wound care, and antibiotics.
Lessons Learned
Although rare, the development of cholecystocutaneous fistula after percutaneous cholecystostomy tube placement is a possible complication. In patients who are poor surgical candidates, a non-operative approach with local wound care and improved nutrition can be implemented to manage these patients.
References
- To H, Brough S, Pande G. Case report and operative management of gallbladder herniation. BMC Surg. 2015;15:72. Published 2015 Jun 11. doi:10.1186/s12893-015-0056-7
- Paolino L, Millan M, Bossi M, Champault G, Barrat C. Herniation of the gallbladder within a hernia of the abdominal wall associated with Mirizzi Syndrome. J Surg Case Rep. 2011;2011(4):3. Published 2011 Apr 1. doi:10.1093/jscr/2011.4.3
- Trotta M, Cesaretti M, Minetti GA, Borgonovo G. Complication of gallbladder herniation through the abdominal wall. Surgery. 2013;154(5):1135-1136. doi:10.1016/j.surg.2012.06.018
- Garcia RM, Brody F, Miller J, Ponsky TA. Parastomal herniation of the gallbladder. Hernia. 2005;9(4):397-399. doi:10.1007/s10029-005-0340-z
- St Peter SD, Heppell J. Surgical images: soft tissue. Incarcerated gallbladder in a parastomal hernia. Can J Surg. 2005;48(1):46.
- Rashid M, Abayasekara K, Mitchell E. A case report of an incarcerated gallbladder in a parastomal hernia. Int J Surg. 2010;23(2):8.
- Shirahama M, Onohara S, Miyamoto Y, Watanabe A, Ishibashi H. Incisional hernia of gallbladder in a patient with gallbladder carcinoma: sonographic demonstration. J Clin Ultrasound. 1997;25(7):398-400. doi:10.1002/(sici)1097-0096(199709)25:7<398::aid-jcu9>3.0.co;2-5
- Sirikci A, Bayram M, Kervancioglu R. Incisional hernia of a normal gallbladder: sonographic and CT demonstration. Eur J Radiol. 2002;41(1):57-59. doi:10.1016/s0720-048x(01)00355-2
- Benzoni C, Benini B, Pirozzi C. Gallbladder strangulation within an incisional hernia. Hernia. 2004;8(4):387-388. doi:10.1007/s10029-004-0220-y
- Goldman G, Rafael AJ, Hanoch K. Acute acalculous cholecystitis due to an incarcerated epigastric hernia. Postgrad Med J. 1985;61(721):1017-1018. doi:10.1136/pgmj.61.721.1017
- McKay A, Abulfaraj M, Lipschitz J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc. 2012;26(5):1343-1351. doi:10.1007/s00464-011-2035-0
- Molavi I, Schellenberg A, Christian F. Clinical and operative outcomes of patients with acute cholecystitis who are treated initially with image-guided cholecystostomy. Can J Surg. 2018;61(3):195-199. doi:10.1503/cjs.003517
- Byrne MF, Suhocki P, Mitchell RM, et al. Percutaneous cholecystostomy in patients with acute cholecystitis: experience of 45 patients at a US referral center. J Am Coll Surg. 2003;197(2):206-211. doi:10.1016/S1072-7515(03)00143-1
- Smith TJ, Manske JG, Mathiason MA, Kallies KJ, Kothari SN. Changing trends and outcomes in the use of percutaneous cholecystostomy tubes for acute cholecystitis. Ann Surg. 2013;257(6):1112-1115. doi:10.1097/SLA.0b013e318274779c
- Dimou FM, Riall TS. Proper Use of Cholecystostomy Tubes. Adv Surg. 2018;52(1):57-71. doi:10.1016/j.yasu.2018.03.011
- Vasanth A, Siddiqui A, O'Donnell K. Spontaneous cholecystocutaneous fistula. South Med J. 2004;97(2):183-185. doi:10.1097/01.SMJ.0000051150.63130.E8
- Hariharan D, Lobo DN. Spontaneous extrusion of gallstones after percutaneous drainage. Ann R Coll Surg Engl. 2017;99(3):e1-e2. doi:10.1308/rcsann.2017.0015
- Rinzivillo NMA, Danna R, Leanza V, et al. Case report: spontaneous cholecystocutaneous fistula, a rare cholethiasis complication. F1000Res. 2017;6:1768. Published 2017 Sep 27. doi:10.12688/f1000research.12235.1
Authors
Narvaez Va; Lin Aa; Kapil Aab; Kartiko Sac
Author Affiliations
- UMass Medical School-Baystate Medical Center, Springfield, MA 01199
- Yale University Medical Center, New Haven, CT 06510
- George Washington University Hospital, Washington, DC 20037
Corresponding Author
Vincent Narvaez, MD
Department of Surgery UMass Medical School-Baystate Medical Center
759 Chestnut Street
Springfield, MA 01199
Phone: (562) 343-8014
Email: vincentreginald.narvaezmd@baystatehealth.org
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: September 2, 2020
Accepted: March 25, 2021