Discussion
Bullet embolization is a rare complication of gunshot wounds. Studies from the military have shown rates from 0.3 to 1.1%.1,2 Embolization to the heart, great vessels, and distal extremities has been well published, however, embolization from a lower extremity to the brain has not previously been described.3,4 A trend appreciated during our literature review showed that most bullet emboli are from close range shotgun blasts. The close range allows for penetration of multiple bullet pellets into the soft tissue giving a greater chance of one of these projectiles to enter into the vascular channels. The surface of the bullets is usually smooth and spherical in shape allowing for easy travel throughout the vascular system. There have been cases describing stroke secondary to bullets from gunshot wounds to the neck, chest, and upper extremities, however, this to our knowledge, is the first documented instance of a lower extremity bullet causing embolic stroke.
Given that the bullet was able to traverse from the systemic venous system and into the arterial system without becoming lodged in the pulmonary vasculature, our patient must have had a patent foramen ovale (PFO). Occult PFO prevalence has been observed in 20 to 30% of patients in autopsy studies.5,6 The patient did undergo a transthoracic echocardiogram (TTE) with agitated saline bubble study, which demonstrated no interatrial shunt; however, there is a known rate of false-negative bubble studies. TTEs are often unable to directly visualize a PFO, but the presence of a PFO can be concluded based on visualization of bubbles within the left atrium.7 The right to left atrial shunt can also be intermittent in nature, and the inability of a patient to appropriately perform a Valsalva maneuver during time of study can further lead to false negative studies.7 One study noted a 35% rate of shunting on TTE with bubble study, with 48% of these only being appreciated after maneuvers, such as Valsalva, which increase intrathoracic pressure and therefore increase right atrial pressure over that of left atrial pressure, thus causing shunting.8 As our patient was intubated at time of TTE, no Valsalva maneuver was able to be performed. Mechanical ventilation itself has been shown to increase intrathoracic pressure enough to cause right to left atrial shunting and identification of a PFO on TTE—but a certain threshold of pressure must still be reached.9 The possibility does exist that other maneuvers during initial evaluation or resuscitation, such as bag-valve-mask ventilation, may have caused sufficient increase in intrathoracic pressure to cause temporary shunting that may have led to the bullet crossing into the arterial system.
Although the literature for covered stent repair for proximal lower extremity injuries is limited, published data does report reasonable outcomes with some advantages over open repair in select patients.9,10 While comparative studies show an advantage of native tissue bypass as compared to stenting in distal peripheral vascular disease, long-term studies of the use of stents in vascular injuries are evolving. Given that this patient’s injury was in a proximal vessel, the segment of occlusion was a short dissection, and there was a large destructive soft tissue defect from the multiple shotgun pellets, we elected to perform the less invasive endovascular intervention (covered stent placement). We do believe that in select patients, stenting proximal vascular injuries does afford patients certain advantages over open repair, such as decreased operative time, decreased blood loss, decreased recovery time, and overall decreased morbidity.
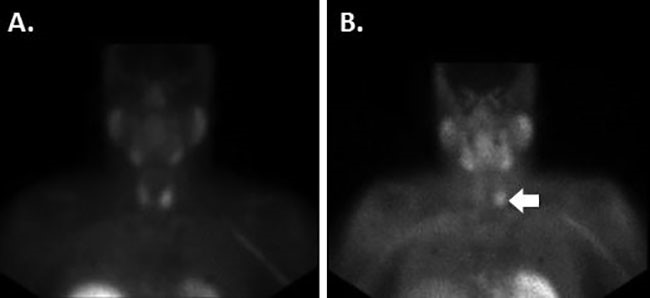
A CT of the head and neck for this intubated patient would have identified the embolization of the bullet with the initial trauma evaluation and prompt treatment likely would have saved the patient from an ischemic stroke and its sequelae. Previous observational and retrospective studies have shown outcome and mortality benefits to whole body CT (WBCT) scans12,13; however, more recent studies, including randomized control trials such as the REACT-2 trial, have shown no difference in 24-hour mortality (8% in the intervention group versus 6% in the control group, p = 0.23), 30-day mortality (17% in the intervention group versus 16% in the control group, p = 0.69), or all patient mortality (15.9% in the intervention group versus 15.7 in the control group, p = 0.92).14,15
Conclusion
We present a patient who presented with a single gunshot wound to the left lower extremity with multiple retained foreign bodies. The patient’s hospital course was complicated by embolization of a bullet to the left MCA resulting in stroke and significant morbidity. This, to our knowledge, is the first documented instance of a lower extremity bullet causing an embolic stroke.
Lessons Learned
Bullet embolization, particularly to the brain, is a rare phenomenon. Based on final location after embolization, neurovascular deficits may be present. Although a gunshot wound may appear localized at first, if there are unaccounted for deficits or a clinical suspicion for embolus, additional imaging should be performed to aid in diagnosis.
Authors
Seyed A. Arshad, MD
Department of Surgery
University of New Mexico School of Medicine
Albuquerque, NM
Andrew C. Christensen, MD
Department of Surgery
University of New Mexico School of Medicine
Albuquerque, NM
Jonathan Marinaro, MD
Division of Emergency Medicine
University of New Mexico School of Medicine
Albuquerque, NM
Sundeep S. Guliani, MD
Department of Surgery
University of New Mexico School of Medicine
Albuquerque, NM
and
Division of Vascular Surgery
University of New Mexico School of Medicine
Albuquerque, NM
Correspondence
Dr. Sundeep S. Guliani
University of New Mexico School of Medicine
Dept Of Surgery- Vascular Division
MSC 10-5610,
1 University of New Mexico
Albuquerque, NM 87131
Phone: 505-272-4531
E-mail: Sguliani@salud.unm.edu
Disclosures
The authors have no conflicts of interest to disclose.
References
- Rich NM, Collins GJ, Andersen CA, Mcdonald PT, Kozloff L, Ricotta JJ. Missile emboli. J Trauma. 1978;18(4):236-9.
- Aidinian G, Fox CJ, Rasmussen TE, Gillespie DL. Varied presentations of missile emboli in military combat. J Vasc Surg. 2010;51(1):214-7.
- Michelassi F, Pietrabissa A, Ferrari M, Mosca F, Vargish T, Moosa HH. Bullet emboli to the systemic and venous circulation. Surgery. 1990;107(3):239-45.
- Elsisi IFHA, Kidambi A. A shot to the heart: a rare case of cardiac embolization. Echo Res Pract. 2018;5(1):K19-K21.
- Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59(1):17-20.
- Meissner I, Whisnant JP, Khandheria BK, et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: the SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin Proc. 1999;74(9):862-9.
- Foo AS, Tan ZK, Lee E, Koh NY. Recurrent episodic hypoxaemic respiratory failure following a stroke. BMJ Case Rep. 2012;2012
- Marriott K, Manins V, Forshaw A, Wright J, Pascoe R. Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. J Am Soc Echocardiogr. 2013;26(1):96-102.
- Vavlitou A, Minas G, Zannetos S, Kyprianou T, Tsagourias M, Matamis D. Hemodynamic and respiratory factors that influence the opening of patent foramen ovale in mechanically ventilated patients. Hippokratia. 2016;20(3):209-213.
- White R, Krajcer Z, Johnson M, Williams D, Bacharach M, O'malley E. Results of a multicenter trial for the treatment of traumatic vascular injury with a covered stent. J Trauma. 2006;60(6):1189-95.
- Stewart DK, Brown PM, Tinsley EA, Hope WW, Clancy TV. Use of stent grafts in lower extremity trauma. Ann Vasc Surg. 2011;25(2):264.e9-13.
- Caputo ND, Stahmer C, Lim G, Shah K. Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;77(4):534-9.
- Surendran A, Mori A, Varma DK, Gruen RL. Systematic review of the benefits and harms of whole-body computed tomography in the early management of multitrauma patients: are we getting the whole picture?. J Trauma Acute Care Surg. 2014;76(4):1122-30.
- Sierink JC, Treskes K, Edwards MJ, et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388(10045):673-83.
- Long B, April MD, Summers S, Koyfman A. Whole body computed tomography versus selective radiological imaging strategy in trauma: An evidence-based clinical review. Am J Emerg Med. 2017.