Figure 3. Chronic Wound Healing Progression. (A) Progression of right and left anterior tibial chronic wound immediately postoperatively, (B) five weeks postoperatively, and (C) final follow-up visit 10 months postoperatively.
Discussion
Graft versus host processes are all too common and create unintended secondary problems in the pursuit of cancer treatment. Skin manifestations can be particularly troublesome, as they may greatly reduce quality of life. Chronic lower extremity wounds are a particularly complex clinical problem, as they accumulate proinflammatory cytokines including tissue necrosis factor-α, Interleukin-1, and neutrophil elastase. Additionally, these cytokines tend to create oxygen radicals that cause senescence of structural dermal elements and cell membranes.6 In this patient, the lower-extremity wound was a result of GVHD and was exacerbated by superficial venous reflux and atherosclerotic disease.
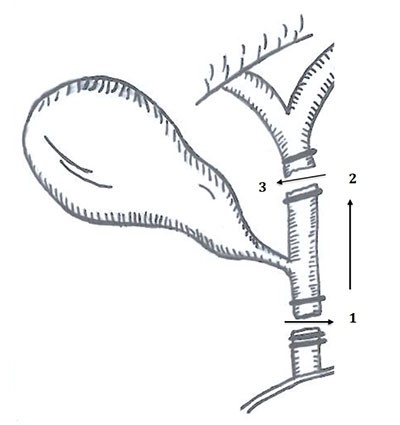
Autologous fat grafting (AFG) has numerous aesthetic and reconstructive applications, yet it has not been described in the treatment of GVHD. Subcutaneous fat has several properties that make it amenable to chronic wound healing; however, its mechanism is still a topic of research. Subcutaneous fat is the largest known depot of multipotent adipose tissue-derived mesenchymal stem cells in the human body.7 As multipotent cells, adipose tissue-derived mesenchymal stem cells have the potential to mature into adipocytes, fibroblasts, mesocytes, and vascular endothelial cells.8 As progenitor cells, adipose tissue-derived mesenchymal stem cells secrete multiple cytokines including vascular endothelial growth factor, placental growth factor, transforming growth factor-β, angiopoietin-1, and fibroblast growth factor-2.8-10 These cytokines aid in tissue regeneration through the promotion of angiogenesis and collagen deposition, even in hypoxic conditions.6,9,10 Furthermore, mesenchymal stem cells express proliferative surface markers for hematopoietic and endothelial cell lineages including CD14, CD34, CD45, and CD144.9 Adipose tissue-derived mesenchymal stem cells also lack human leukocyte antigen-DR expression, which decreases the risk of tissue rejection post-transplantation.8 Interestingly, these stem cells have demonstrated immunosuppressive characteristics that subdue the proliferation of activated lymphocytes in vivo.6,8,11 Therefore, the multipotent, angiogenic, and immunomodulatory effects of ADSCs transplanted in AFG contribute to the treatment of sclerotic chronic GVHD and poor perfusion. Injection of adipocytes in the sclerotic wound periphery provides structural support for mesenchymal stem cells. In addition, multiple passes of the cannula through the sclerotic wound edges mechanically breaks fibrotic tissue and increases the surface area of exposed tissue to mesenchymal stem cells for neovascularization and new collagen deposition.
Autologous fat grafting is a short, single-stage, outpatient procedure with low demands on wound healing, minimal donor site morbidity, and avoidance of flap reconstruction, which would be difficult in a poorly-perfused sclerotic extremity. Potential complications of fat grafting include damage to the viscera, lungs, or surrounding tissues during harvest, infection, subcutaneous contour deformities, donor site pain, necrosis, and need for repeat procedures.12 These complications were not encountered in our patient.
The patient declined biopsy to determine the histologic architecture and composition of the regenerated tissue. However, we believe that the use of autologous fat grafting is safe and effective, and that it helped promote resolution of the previously chronic wounds of the sclerotic chronic GVHD patient. Fat grafting can be considered for carefully-selected patients who are otherwise not ideal surgical candidates. Future studies may aim to replicate these results in a larger population, utilizing pre- and postoperative biopsies to determine histologic changes as a result of AFG.
Conclusion
We report the first case of the successful treatment of chronic lower extremity wounds in a sclerotic chronic GVHD patient with AFG. Knowledge of this safe treatment may help guide difficult management issues that arise in sclerotic chronic GVHD. Further research with control treatments, long-term follow-up, and post-treatment histologic examination is warranted to further develop treatment protocols with AFG for this subset of patients.
Lessons Learned
AFG may be used to treat lower extremity chronic ulceration due to sclerotic chronic GVHD. We present the novel application of autologous fat grafting for treatment of chronic lower extremity wounds as a result of sclerotic chronic graft versus host disease.
Authors
Julia A. Cook, MDa; Sarah E. Sasor, MDa; Steven A. Mann, MDb; Terrence Katona, DOc; Sunil S. Tholpady, MD, PhDa,d; Michael W. Chu, MDe
Correspondence Author
Dr. Julia A. Cook
Indiana University School of Medicine
Division of Plastic & Reconstructive Surgery
545 Barnhill Drive, #232
Indianapolis, IN 46202
email: juacook@gmail.com
phone: (317) 274-5831
fax: (317) 278-8746
Author Affiliations
a Indiana University School of Medicine, Division of Plastic & Reconstructive Surgery
b Indiana University School of Medicine, Department of Pathology and Laboratory Medicine
c R. L. Roudebush Veterans Affairs Medical Center, Department of Pathology and Laboratory Medicine
d R.L. Roudebush Veterans Affairs Medical Center, Division of Plastic & Reconstructive Surgery
e Kaiser Permanente West Lost Angeles Medical Center, Division of Plastic & Reconstructive Surgery
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Shlomchik WD. Graft-versus-host-disease. Nat Rev Immunol. 2007;7:340-352.
- Horwitz ME, Sullivan KE. Chronic graft-versus-host-disease. Blood Rev. 2006;20:15-27.
- Brüggen MC, Klein I, Greinix H, et al. Diverse T-cell responses characterize the different manifestations of cutaneous graft versus host disease. Blood 2014;123:290-299.
- Jagasia MH, Greinix HT, Arora M, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft versus host disease: I, the 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389-401.
- Coleman SR. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19:421-425.
- Fromm-Dornieden C, Koenen P. Adipose-derived stem cells in wound healing: recent results in vitro and in vivo. Mol Cell Biol. 2013;1:8-13.
- Hsu VM, Stransky CA, Bucky LP, Percec I. Fat grafting’s past, present, and future: why adipose tissue is emerging as a critical link to the advancement of regenerative medicine. Aesthet Surg. 2012;32:82-89.
- Schaffler A, Buchler C. Concise review: adipose tissue-derived stromal cells—basic and clinical implications for novel cell-based therapies. Stem Cells. 2007;25:818-827.
- Nakagami H, Morishita R, Maeda K, Kikuchi Y, Ogihara T, Kaneda Y. Adipose tissue-derived stromal cells as a novel option for regenerative cell therapy. J Atheroscler Thromb. 2006;13:77-81.
- Stasch T, Hoehne J, Huynh T, De Baerdemaeker R, Grandel S, Herold C. Debridement and autologous lipotransfer for chronic ulceration of the diabetic foot and lower limb improves healing. Plast Reconstr Surg. 2015;136:1357-1366.
- Le Blanc K, Frassoni F, Ball L, et al. Mesenchymal stem cells for treatment of steroid-resistant severe, acute graft-versus-host-disease: a phase II study. Lancet. 2008;371:1579-1586.
- Luu CA, Larson E, Rankin TM, Pappalardo JL, Slepian MJ, Armstrong DG. Plantar fat grafting and tendon balancing for the diabetic foot ulcer in remission. Plast Reconstr Surg Glob Open. 2016;4:e810.