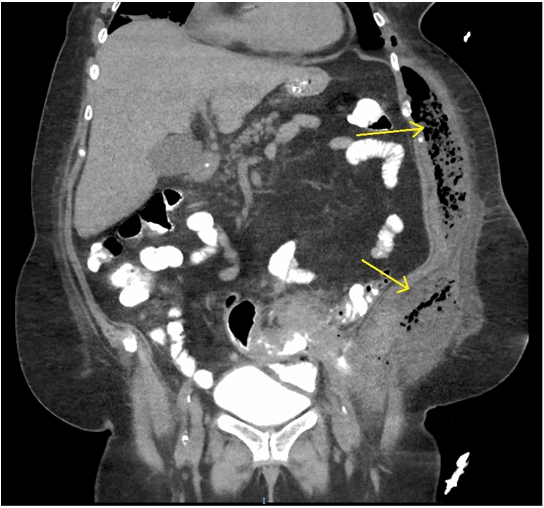
Figure 6. A. Recurrent left sided AVF, prior to stent deployment. Fistula is seen between the common femoral artery and vein. B. Angiogram after stent deployment. Fistula no longer visualized. LCFV=left common femoral vein; LCFA=left common femoral artery.
On the right an 8 mm x 10 cm Viabahn stent-graft was utilized to exclude the recurrent AV fistula and pseudoaneurysm in the common femoral artery. A repeat arteriogram revealed successful repair of the common femoral arteries with adequate distal flow into the bilateral superficial femoral arteries. Following this procedure the patient’s heart failure improved with medical therapy and he was able to resume his rehabilitation. He was eventually discharged home with outpatient therapy. He was seen in clinic several times and was recovering well but unfortunately was lost to follow up from our health system.
Discussion
We present the extremely rare case of traumatic bilateral femoral AVFs, with the added rare example of AVF recurrence resulting in high-output cardiac failure. A high index of suspicion must remain when considering traumatic AVFs, especially in the multisystem injured patient where AVF diagnosis is often delayed due to nonspecific signs and symptoms.6 Time to diagnosis of traumatic AVFs has been found to vary from hours to years.7
Options for repair of lower extremity AVFs include open repair and endovascular techniques. Although open repair can often be performed quickly in cases of acute AVFs, endovascular repair presents a useful option, especially in hemodynamically stable patients, patients at high risk for anesthesia, those with extensive scar tissue in the groin, or patients who may not tolerate hemorrhage that may occur with open surgical repair.1 Typically stent-graft placement is avoided in the common femoral artery due to the risk of stent-graft deformation or fracture from hip flexion or rotation, especially in young, active patients. Furthermore, long-term patency rates are unclear, as many studies have follow-up only to one year.8,9,10 Stent-graft placement at this location also precludes the use of the site for future femoral access.1 Despite these risks, studies have shown successful treatment of lower extremity AVFs with endovascular stenting.1 In our case, the patient was taken to interventional radiology due to the concern of ongoing pelvic bleeding, without an initial suspicion of AVF. Once discovered on angiogram, after discussion between radiology and surgery, the decision was made to proceed with endovascular repair in order to minimize further delays given the patient’s critical state. The recurrence of the bilateral AVFs due to endovascular leak and pseudoaneurysm formation in our patient underscores the importance of ongoing surveillance and monitoring in patients with proximal lower extremity stent-grafts in order to ensure long-term success. Further studies are needed to assess the long-term sequelae and success of proximal lower extremity stent-grafts.
Another important consideration if traumatic AVF is suspected and endovascular repair is to be performed, is treatment in an operating room with endovascular capabilities. In our case, AVF was not suspected at the time the decision was made to proceed to interventional radiology. However, treatment delay did occur once difficulties with access to the right superficial femoral artery were encountered in interventional radiology requiring transfer to an operating room. If available, an operating room with endovascular capabilities provides a broader range of flexibility, as endovascular and/or open surgical techniques can be performed, including thromboembolectomy and four-compartment fasciotomy, as required in the case of our patient.
Finally, our patient not only acquired bilateral femoral AVFs, but also suffered from the rare complication of high-output cardiac failure. Although often described as a hemodynamic complication of AVFs,12 this phenomenon is infrequently reported in the literature.3,4,13,14 Presentation is variable, with signs and symptoms ranging from atrial fibrillation, lower extremity edema, dyspnea, or tachycardia and activity intolerance, as in the case of our patient. Furthermore, cardiac failure can occur at a range of post-trauma times, within weeks, as in our case, up to 63 years.14 Again, this highlights the importance of ongoing follow-up in patients suffering from traumatic AVF.
Conclusion
Traumatic AVF is a relatively infrequent occurrence. We present the rare case of traumatic bilateral femoral AVF with recurrence after endovascular repair due to endoleak and pseudoaneurysm formation as well as high-output cardiac failure. Prompt evaluation and treatment of the AVF is crucial. Endovascular repair has been reported to be successful in lower extremity AVF. Endovascular repair was ultimately successfully performed in our patient and appears to be a safe option in management of traumatic AVF. However long-term follow-up is important in order to monitor for complications due to the potential for stent-graft failure.
Lessons Learned
Traumatic AVFs are a relatively rare occurrence, especially in the extremities. A high index of suspicion must remain when considering AVFs, especially in the multisystem injured trauma patient where diagnosis of an AVF can be delayed due to nonspecific signs and symptoms. High-output cardiac failure is a known potential complication of AVFs, but it is infrequently reported in the literature. Again, a high index of suspicion must remain due to its varying presentation and time-course.
Authors
Shah M, Puzio T, Marston W, Johnson DL
Correspondence Author
Daryhl Johnson MD, MPH, FACS
Department of Surgery
University of North Carolina
4008 Burnett Womack Building
CB 7228
Chapel Hill, NC 27516
919-966-4389
daryhl_johnson@med.unc.edu
Author Affiliations
Department of Surgery
University of North Carolina
Chapel Hill, NC
References
- Mohler ER III. Acquired arteriovenous fistula of the lower extremity. UpToDate, Clement DL, Eidt, JF, Mills Sr, JL (Eds), UpToDate, Waltham, MA. (Accessed on April 10, 2016).
- http://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/venous-disorders/arteriovenous-fistula. Accessed: April 10, 2106
- Hüseyin S, Yüksel V, Güçlü O, Canbaz S. A Rare Etiology of Heart Failure: Traumatic Arteriovenous Fistula Due to Stab Injury 17 Years Ago. Balkan Med J. 2015 Jul; 32(3): 309–311. doi: 10.5152/balkanmedj.2015.15291
- Trindade VD, Piantá RM, Heck AA, Goldani MA. High-output heart failure resulting from a traumatic arteriovenous fistula. J Vasc Surg. 2015 May;61(5):1329. doi: 10.1016/j.jvs.2014.01.075.
- Chiriac A, Iliescu BF, Dobrin N, Poeata I. One-step endovascular treatment of bilateral traumatic carotid-cavernous fistulae with atypical clinical course. Turk Neurosurg. 2014;24(3):422-6. doi: 10.5137/1019-5149.JTN.8004-13.1.
- Roth P, Heiss C, Koshty A, Niemann B, Boening A. Posttraumatic Arteriovenous Fistula of the Distal Posterior Tibial Artery as Cause of Delayed Wound Healing in an Unrecognized Arterial Injury. Thorac Cardiovasc Surg Rep. 2014 Dec; 3(1): 67–70. doi: 10.1055/s-0033-1363167
- Baril DT, Denoya PI, Ellozy SH, et al. Endovascular repair of a traumatic arteriovenous fistula 34 years after the injury: report of a case. Surg Today. 2007;37(1):78-81
- Thalhammer C, Kirchherr AS, Uhlich F, Waigand J, et al. Postcatheterization pseudoaneurysms and arteriovenous fistulas: repair with percutaneous implantation of endovascular covered stents. Radiology. 2000;214(1):127.
- Baltacioğlu F, Cimșit NC, Cil B, et al. Endovascular stent-graft applications in latrogenic vascular injuries. Cardiovasc Intervent Radiol. 2003;26(5):434.
- Waigand J, Uhlich F, Gross CM, et al. Percutaneous treatment of pseudoaneurysms and arteriovenous fistulas after invasive vascular procedures. Catheter Cardiovasc Interv. 1999;47(2):157.
- Rogel-Rodríguez JF, Zaragoza-Salas T, Díaz-Castillo L, et al. posttraumatic femoral arteriovenous fistula, endovascular treatment. Cir Cir. 2016 Jan 4. doi: 10.1016/j.circir.2015.10.010.
- Wilson SE. Vascular Access: Principles and Practice, 5th edition. Philadelphia: Lippincott Williams and Wilkins, 2010.
- Vagefi, PA, MD, Kwolek, CJ, MD, Wicky, S, MD, Watkins, MT MD. Congestive heart failure from traumatic arteriovenous fistula. J Am Coll Surg. 2009 Jul;209(1):150. doi: 10.1016/j.jamcollsurg.2008.11.021
- Frishman W, Epstein AM, Kulick S, Killip T. Heart failure 63 years after traumatic arteriovenous fistula. Am J Cardiol. 1974 Nov;34(6):733-6.