Figure 5. Follow-up chest X ray of patient with Transmediastinal gunshot wound. Solid yellow line indicates the position of the bullet on X ray.
Conclusion
In this case of a hemodynamically stable patient with a transmediastinal gunshot wound, given the patient's clinical stability evaluation using CT, pericardial window, endoscopy and bronchoscopy allowed us to rule out clinically significant mediastinal injury without a more morbid surgical exploration.
Lessons Learned
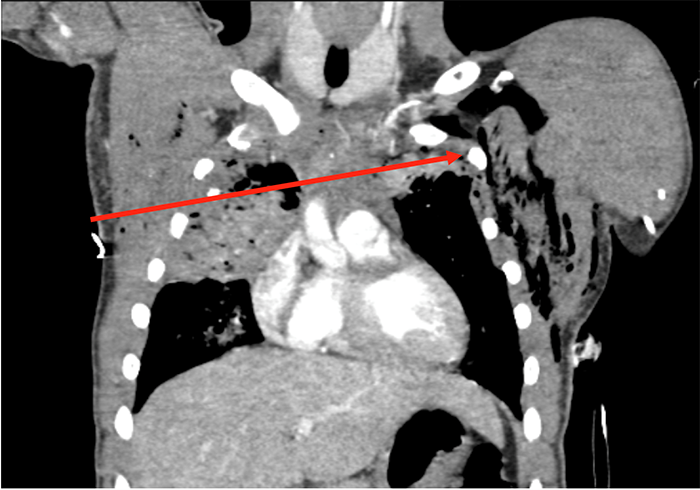
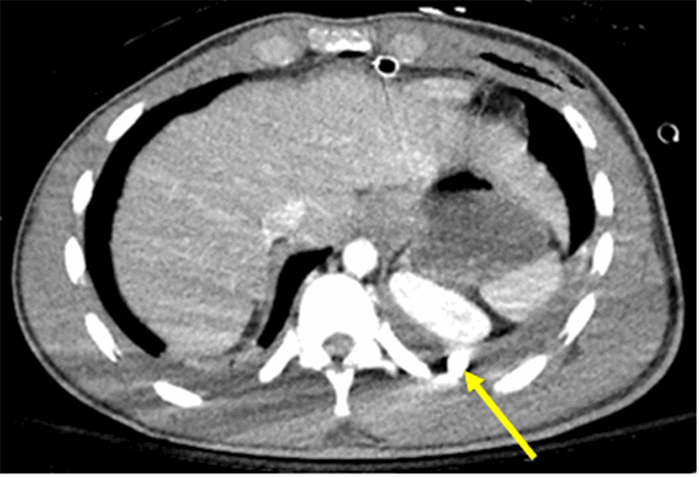
While implied trajectory on X rays can suggest injury patterns and guide further investigation, it is important to remember that bullets do not always follow linear paths. In particular, bullets can migrate freely in the pleural space in the context of a hemopneumothorax.
Authors
Adam D. Laytin, MD, MPH
Division of Traumatology, Surgical Critical Care & Emergency Surgery
Department of Surgery
University of Pennsylvania; Philadelphia, PA
Michael A. Vella, MD, MBA
Division of Traumatology, Surgical Critical Care & Emergency Surgery
Department of Surgery
University of Pennsylvania; Philadelphia, PA
Jose L. Pascual, MD, PhD, FACS
Division of Traumatology, Surgical Critical Care & Emergency Surgery
Department of Surgery
University of Pennsylvania; Philadelphia, PA
Niels D. Martin, MD, FACS
Division of Traumatology, Surgical Critical Care & Emergency Surgery
Department of Surgery
University of Pennsylvania; Philadelphia, PA
Correspondence Author
Niels D. Martin, MD, FACS, FCCM
Division of Traumatology, Surgical Critical Care & Emergency Surgery
Perelman School of Medicine at the University of Pennsylvania
51 North 39th St, Medical Office Building Suite 120
Philadelphia, PA 19104
Phone: 215-662-7323
Email: Niels.Martin@uphs.upenn.edu
Disclosure Statement
Conflicts of Interest and Source of Funding: No author has a conflict of interest, competing interest or financial disclosure to declare. All authors have met criteria for authorship and ethical adherence. There were no sources of funding for this project.
References
- Nagy KK, Roberts RR, Smith RF, Joseph KT, An GC, Bokhari F, Barrett J. Transmediastinal gunshot wounds: are "stable" patients really stable? World J Surg. 2002;26(10):1247-50.
- Stassen NA, Lukan JK, Spain DA, Miller FB, Carrillo EH, Richardson JD, Battistella FD. Reevaluation of diagnostic procedures for transmediastinal gunshot wounds.J Trauma. 2002;53(4):635-8; discussion 8.
- Ibirogba S, Nicol AJ, Navsaria PH. Screening helical computed tomographic scanning in haemodynamic stable patients with transmediastinal gunshot wounds. Injury. 2007;38(1):48-52.
- Karmy-Jones R, Namias N, Coimbra R, Moore EE, Schreiber M, McIntyre R, Jr., Croce M, Livingston DH, Sperry JL, Malhotra AK, et al. Western Trauma Association critical decisions in trauma: penetrating chest trauma. J Trauma Acute Care Surg. 2014;77(6):994-1002.
- Treto K, Bhullar IS, Lube MW. Iliac Artery Bullet Embolus after Isolated Thoracic Ballistic Injury. Am Surg. 2017 Jul 1;83(7):e253-254.
- Hughes JJ. Bullet injury to the esophagus detected by intestinal migration. J Trauma. 1987 Dec;27(12):1362-4.
- Davis RE, Bruno AD, Larsen WB, Sugimoto JT, Gaines RD. Mobile intrapericardial bullet: case report and review of the literature. J Trauma. 2005 Feb;58(2):378-80.
- Todnem N, Hardigan T, Banerjee C, Alleyne CH. Cephalad Migration of Intradural Bullet from Thoracic Spine to Cervical Spine. World Neurosurg. 2018;119:6-9.
- Mowery NT, Gunter OL, Collier BR, Diaz JJ, Jr., Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011;70(2):510-8.
- Kirkpatrick AW, Rizoli S, Ouellet JF, Roberts DJ, Sirois M, Ball CG, Xiao ZJ, Tiruta C, Meade M, Trottier V, et al. Occult pneumothoraces in critical care: a prospective multicenter randomized controlled trial of pleural drainage for mechanically ventilated trauma patients with occult pneumothoraces. J Trauma Acute Care Surg. 2013;74(3):747-54; discussion 54-5.
- Williams CG, Haut ER, Ouyang H, Riall TS, Makary M, Efron DT, Cornwell EE. Video-assisted thoracic surgery removal of foreign bodies after penetrating chest trauma. J Am Coll Surg. 2006;202(5):848-52.