Abstract
Background
Long-term venous access ports are used for patients with chronic ailments, allowing providers access to veins for parenteral nutrition, medications, and blood draws. Here, we provide a rare example of the misplacement of a catheter into the epidural space of a patient's spinal cord.
Summary
Placement of long-term venous access ports is not without risk of complications. Here, we report a rare misplacement of internal jugular chemo-port into the epidural space. A port contrast study by an interventional radiologist confirms the port's location in the epidural space. The port was immediately removed, and the patient recovered uneventfully.
Conclusion
Although venous access ports are widely used, they are not without risk for complications, both when being placed and with usage. Complications can include venous misplacement of the catheter, pneumothorax, infection, and embolization of the catheter. A high index of suspicion should be maintained for this complication due to the significant morbidity and mortality associated with this complication.
Key Words
complications; delayed complications
Case Description
A two-year-old female with a past medical history of cystic fibrosis, exocrine pancreatic insufficiency, and failure to thrive presented to the pediatric surgical service for the placement of a central venous catheter (CVC) chemo-port after multiple episodes of cystic fibrosis exacerbations and poor venous access. Of note, the patient has no previous history of neck surgery or vascular access in the neck.
She was taken to the operating room for a routine chemo-port placement. A right internal jugular chemo-port was placed using ultrasound guidance. The venous placement was confirmed by fluoroscopy in the operating room; no vascular abnormality was noted on fluoroscopy. Blood was able to be aspirated from the port, and the port was able to be flushed postoperatively. The catheter appeared more medial than usual, but the patient's lung disease had slightly displaced her heart to the left. Due to little difficulty encountered during any of the stages of the procedure and the port appearing to be functional at the end of the procedure, there was no concern about procedure-related complications at that time.
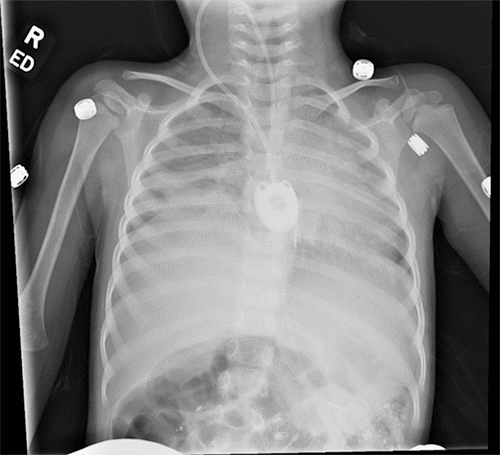
After the procedure, a chest X ray (Figure 1) confirmed the seemingly successful placement of the CVC chemo-port; the patient was transferred to the pediatrics team for postoperative monitoring. Over the next few days, the port never functioned correctly. A minimal amount of blood was able to be aspirated from the port. While it seemed to flush well, the patient would complain of severe pain when normal saline flush was injected through the port. The pain was described as being all over her body. She could not be distracted from the pain, which reportedly stopped as soon as the flush was stopped. Although no IV medication was ever administered through the port, injection of TPA was performed through the port due to a concern of sluggish blood draw from the port, which did not improve with a blood draw. Due to concern for a malpositioned port, interventional radiology was consulted and performed a port contrast study (Figure 2 and Figure 3) which revealed that the catheter was located in the epidural space, which was confirmed by a CT scan (Figure 4). The port was immediately removed while the patient was sedated in the radiology suite.
Figure 1. Postoperative Chest X Ray. Published with Permission
Figure 2. Beginning of Port Study. Published with Permission
Figure 3. Contrast in Epidural Space. Published with Permission
Figure 4. CT Confirmation of Epidural Space Displacement. Published with Permission
She was monitored in the ICU overnight with frequent neurovascular checks. Postoperatively, neurosurgery was also consulted, and no additional workup/intervention was recommended as the patient recovered uneventfully back to her normal baseline.
Discussion
Central venous access ports play an important role in the management of patients with chronic ailments. Its usage ranges from administering intravenous medication and nutritional therapy to withdrawing blood.1 The placement of these ports involves percutaneously accessing one of the veins in the neck, subclavian, or internal jugular vein, under ultrasound guidance. Once the central venous system is accessed, the port and its associated catheter are placed under fluoroscopic guidance. Despite advances in medical equipment and imaging, port placement-related complications are not uncommon. Immediate complications include vascular injury, cardiac injury, pulmonary injury, and misplacement of the port.2 Delayed complications include device dysfunction, thrombosis, and infection.2
Misplacement of a port happens when the catheter portion of the port is not located inside the SVC at the atriocaval junction. Anatomic variations such as stenosis/occlusion of the vessel, angulation of the vessel, congenital variation, and error in judgment by the surgeon are some risk factors for this complication.3 A misplacement of the port can often be classified into two types (intracava and extracava), depending on the final location of the catheter portion of the port. The intracava misplacement includes placement of the port into the carotid artery,4 azygos vein,5 internal mammary vein,6 or vertebral vein.7 Chest X ray often identifies the intracava misplacement of the port readily. It is often managed successfully by the immediate removal of the port under radiographic guidance.
The less common type of port misplacement is the misplacement of the port into the extra-cava space, which includes the epidural space,8 the pericardium,9 the pleural space, the mediastinum10 or the thoracic duct. This complication is often associated with significant morbidity and mortality in the scant case reports on the topic. In our case report, the port was noted to have been misplaced into the epidural space. To our knowledge, only two other case reports previously reported the misplacement of a central venous catheter into the epidural space.8,11 The first case reported the presence of iatrogenic epidural hematoma following the placement of a central venous catheter via the right internal jugular vein.8
Like our case, the chest X ray following the central catheter placement appeared to be in an optimal position. However, on postoperative day 2, the patient was noted to develop marked swelling around his neck. CT imaging showed the catheter tip had penetrated the jugular vein and entered the intervertebral foramen, reaching the spinal epidural space. Unfortunately, the patient developed epidural hematoma following the removal of the catheter, requiring emergent surgical decompression. Similarly, the second case reported a misplacement of the central venous catheter into the epidural space.11 In this particular case, the central venous catheter was placed for the administration of chemotherapy. The postprocedural chest X ray showed that the catheter tip is in the midline, presumably in the correct position. Subsequently, the patient received chemotherapy through this central venous catheter. After several weeks, the patient developed vomiting, back pain, and weakness in the lower extremities. The symptoms worsened, and the patient died six days after hospital admission due to brain stem toxicity.
The rarity of this complication, the age of the patient, the size of the blood vessel, the inability to detect incorrect placement of the port, and the port being able to be aspirated and flushed were some of the causes that led to the delay in diagnosis of misplacement of port in our case. The most important learning point from our case is to have an initial high index of suspicion for the misplacement of the port, especially in the setting of an abnormal position of the catheter on imaging at the end of the case. However, we were fortunate that the patient recovered to her normal baseline, and no long-term sequelae was noted. Making the diagnosis earlier intraoperatively would have prevented the pain associated with infusion through the catheter and prevented an additional procedure requiring sedation. Examining the wire and the tip of the catheter for movement with cardiac motion during insertion and/or performing an intraoperative contrasted study are some things we will do in the future intraoperatively when there is a concern for the misplacement of the port on imaging.
Conclusion
Placement of long-term venous access ports is not without risks for complications. Due to the rarity of this complication, timely diagnosis of this complication may be challenging. A high index of suspicion should be maintained for this complication due to the significant morbidity and mortality associated with this complication. Diagnostic test, such as immediate intraoperative contrasted port study, helps identify this complication.
Lessons Learned
Complications associated with central venous port placement into the extracava space, specifically into the epidural space, are rare. Despite its rarity, a high index suspicion of misplacement of the central venous port should always be maintained due to the potential severity of morbidity and mortality associated with this complication. From our experience, we recommend an immediate intraoperative contrasted port study if there is any concern for misplacement of the port.
Authors
Budi Sa; Calick Db, Parrish Da
Author Affiliations
- West Virginia University Community Medicine, Morgantown, WV 26506
- West Virginia University School of Medicine, Morgantown, WV 26506
Corresponding Author
Daniel Calick, MD
Department of Emergency Medicine
Virginia Tech Carilion
1 Riverside Circle
Roanoke, VA 24016
Email: danielcalick@yahoo.com
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: September 28, 2020
Revision received: November 9, 2020
Accepted: December 7, 2020
References
- McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):1123-1133. doi:10.1056/NEJMra011883
- Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular versus subclavian access--a systematic review. Crit Care Med. 2002;30(2):454-460. doi:10.1097/00003246-200202000-00031
- Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 2011;4:27-39. doi:10.2147/RMHP.S10383
- Kaitzis DG, Balitas AG, Skandalos IK, Hatzibaloglou AK. Carotid artery repair after erroneous insertion of a hemodialysis catheter: case report. J Vasc Access. 2006;7(3):136-138. doi:10.1177/112972980600700309
- Bankier AA, Mallek R, Wiesmayr MN, et al. Azygos arch cannulation by central venous catheters: radiographic detection of malposition and subsequent complications. J Thorac Imaging. 1997;12(1):64-69. doi:10.1097/00005382-199701000-00010
- Ghafoor H, Fatimi Sh, Ali M. Unusual malposition of dialysis catheter in the left internal mammary vein--a case report. Middle East J Anaesthesiol. 2011;21(1):139-141.
- Yang SH, Jung SM, Park SJ. Misinsertion of central venous catheter into the suspected vertebral vein: a case report. Korean J Anesthesiol. 2014;67(5):342-345. doi:10.4097/kjae.2014.67.5.342
- Orme RM, McSwiney MM, Chamberlain-Webber RF. Fatal cardiac tamponade as a result of a peripherally inserted central venous catheter: a case report and review of the literature. Br J Anaesth. 2007;99(3):384-388. doi:10.1093/bja/aem181
- O'Sullivan P, Brown M, Hartnett B, Mayo JR. Central line pump infusion and large volume mediastinal contrast extravasation in CT. Br J Radiol. 2006;79(944):e75-e77. doi:10.1259/bjr/30451779
- Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Kuroiwa T. Spinal epidural hematoma following removal of incorrectly placed jugular central venous catheter. J Neurosurg Spine. 2011;15(2):206-209. doi:10.3171/2011.3.SPINE10900
- Paralta Branco F, Brito CB, Luz G, Teixeira JA. Central venous catheter misplaced in the epidural space. BMJ Case Rep. 2019;12(4):e229295. Published 2019 Apr 8. doi:10.1136/bcr-2019-229295