Abstract
Background
A 77-year-old male underwent placement of a dual-lead permanent pacemaker via his left subclavian vein. Immediate postoperative chest X ray (CXR) was negative for pneumothorax (PTX), and pacemaker interrogation studies were adequate, so he was discharged home the same day.
Summary
Our facility has been practicing same-day discharges for pacemakers if their postoperative CXR is negative and if pacemaker parameters are acceptable a few hours after surgery. The patient has obstructive sleep apnea and uses a continuous positive airway pressure (CPAP) mask at night. On postoperative day 5, he returned to the emergency department with shortness of breath. CXR then showed a large left PTX with mediastinal shift but no tension physiology. A left chest tube was placed and resolved the PTX, but subsequent interrogation of his pacemaker leads suggested that the ventricular lead had become dislodged from the myocardium. We took him back to the operating room for the replacement of the ventricular lead. The patient did well postoperatively, his chest tube was removed, and he was discharged a few days later.
Conclusion
Extra caution is needed in CPAP-dependent patients who undergo thoracic procedures such as pacemakers, ports, lung biopsies, and thoracenteses. The positive pressure from the CPAP can turn a small undetectable pneumothorax into a delayed pneumothorax several days later. Mediastinal shift, which is rapidly reversed after chest tube placement, can dislodge pacemaker leads. We suggest observing CPAP patients for a night after any procedure that requires instrumentation of their central venous system to ensure that delayed pneumothorax does not develop.
Key Words
delayed complication; tension physiology; lung injury
Abbreviations
Continuous positive airway pressure: CPAP
Chest X ray: CXR
Pneumothorax: PTX
Right ventricle: RV
Case Description
The patient in this case report is a 77-year-old male with a history of type 2 diabetes, hypertension, and obstructive sleep apnea treated with a nightly continuous positive airway pressure (CPAP) mask. He presented to our local emergency department with new onset dizziness and chest palpitations. He was evaluated and was found to have a complete third-degree heart block. Cardiology recommended the placement of a permanent dual-chamber cardiac pacemaker. General surgeons place pacemakers at our institution, and the devices are programmed and tested by a technologist employed by the device manufacturer.
The patient was brought back to the operating room for placement of a dual chamber pacemaker via his left subclavian vein under monitored anesthesia care. The vein was accessed on the first attempt using anatomic landmarks. But, with the patient under monitored anesthesia care, it was not possible to have him hold his breath as the needle was inserted. There were no issues when we were threading the guidewires. We made a few adjustments with the right ventricle (RV) lead to find a suitable location for lead placement, but overall it was a routine pacemaker procedure. A portable chest X ray (CXR) was obtained about 15 minutes later in the recovery room and was negative for pneumothorax (PTX) (Figure 1). About three or four hours later, the pacemaker technologist interrogated the device, and all parameters were appropriate, so the patient was discharged home. Our institution had been moving toward same-day discharges unless there were other reasons to keep the patient overnight, but this patient lived nearby and was comfortable with discharge.
Figure 1. Immediate Postoperative Chest X Ray (CXR). Published with Permission
The patient went home and was doing well for the next several days. He wears a standard CPAP mask at night and has been doing so for several years. On the morning of postoperative day 5, he woke up with severe shortness of breath. He returned to the emergency department. In the ED, his vitals were normal, and he maintained oxygen saturation above 90% on nasal cannula. CXR demonstrated a large left pneumothorax with a left-to-right mediastinal shift (Figure 2). The surgery team was consulted at this time and placed a 20 Fr chest tube into the left chest with an evacuation of a significant amount of air. Even though he had a mediastinal shift, he had not yet developed tension physiology. Postprocedure CXR demonstrated resolution of the PTX, but the ventricular pacemaker lead appeared out of place (Figure 3). With no history of chronic obstructive lung disease or prior imaging suggestive of blebs, we concluded that this PTX was most likely a technical complication of our left subclavian vein cannulation.
Figure 2. Left Pneumothorax (PTX) on Postoperative Day 5. Published with Permission
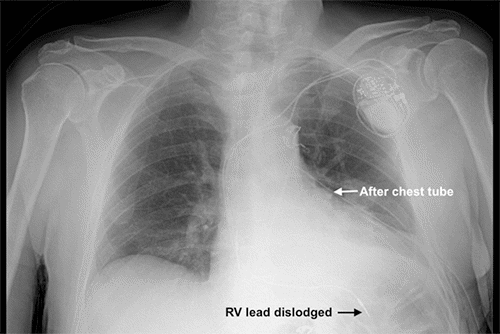
Figure 3. Resolution of PTX After Left Chest Tube Placement. Published with Permission
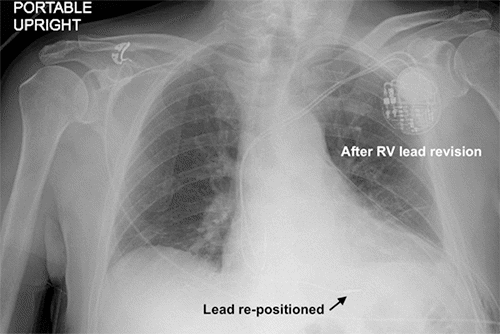
The patient's dyspnea resolved, but he developed the same type of heart palpitations and dizziness that he had been experiencing before his pacemaker. His pacemaker was interrogated, and it was not possible to stimulate the ventricular lead, suggesting that the lead was free-floating in the ventricle. We concluded that the lead had been pulled out by the rapid reversal of his mediastinal shift after placing the chest tube. The patient was brought back to the operating room the next day to reposition the lead into the myocardium of the apical septum of the RV. His chest tube was water sealed and removed the following day. We had him use his CPAP overnight and confirmed no PTX 24 hours after chest tube removal. He was discharged home in stable condition and was doing well with no recurrent PTX at follow-up a week later.
Figure 4. Repositioning of RV Pacemaker Lead. Published with Permission
Discussion
In this case report, we present a 77-year-old male who had two complications related to permanent cardiac pacemaker placement. He developed a delayed pneumothorax, which we suspect was caused by a small iatrogenic lung injury during his pacemaker placement and was then propagated over the next few days by the positive pressure from his CPAP. His second complication was the dislodgement of the RV pacemaker lead. The lead likely was dislodged by the rapid reversal of the mediastinal shift once the chest tube was placed. An alternative but less likely explanation is that the lead was pulled out gradually by the development of the mediastinal shift as his PTX was developing. Still, we have no evidence of pacemaker abnormalities before his chest tube was placed. Lead dislodgement secondary to tension PTX has been described before,1 as, too, have spontaneous pneumothoraces secondary to CPAP.2 However, this is the first known report of both complications occurring together, and it provides several valuable lessons that can improve how we care for these patients.
Pneumothorax is a known complication from pacemaker placement, with an incidence of around 0.9% to 1.2%.3 It is more common after subclavian approaches compared to the internal jugular route, and its incidence can be decreased further if ultrasound guidance is used (0.5% to 2% versus 0.2% to 0.5%).4 Multiple attempts at cannulating the subclavian vein also increase the risk of PTX.5 Post-procedure CXR is the routine method to rule out immediate PTX after procedures that access the central veins or chest cavity (central lines, pacemakers, lung biopsies, thoracenteses, etc.), although the sensitivity of CXR at detecting occult pneumothoraces has been debated.4
Spontaneous pneumothoraces caused by positive airway pressure therapy for sleep apnea have also been described2,6 as have pneumothoraces in patients who are endotracheally intubated.7,8 A significant risk factor is diseased or injured lungs. Even though our initial postoperative CXR was negative for PTX, it was taken only several minutes after surgery. This is probably not enough time for a PTX to develop, especially since he had not yet spent a night on CPAP.
Lead dislodgement is a known complication after cardiac rhythm device placement (pacemakers, defibrillators, and cardiac resynchronization devices), occurring in about 1.4% of cases. It usually gets diagnosed early, before the patient is discharged. The right atrial lead is more likely to get dislodged than the right ventricular lead.9 There is one other case report1 that describes lead dislodgement from tension PTX. In that report, the PTX was first diagnosed 48 hours postoperatively before the patient was discharged from the hospital.
This is the first report of a delayed PTX from a pacemaker in the setting of CPAP therapy. We suspect the subclavian cannulation must have caused a slight lung injury when his pacemaker was placed. In a patient not on CPAP therapy, this likely would not have turned into a significant PTX. But since our patient was receiving positive pressure to his airways, he likely slowly built up pleural air for days and was about to develop tension physiology when he returned to our ED. Our facility had been working on a protocol for same-day discharge for pacemakers. Still, this case represents a potentially dangerous setup for patients if we discharge patients home without observing how their pleural space will respond to a night of CPAP therapy. An extra day of observation and a postoperative day 1 CXR might benefit high-risk patients such as those with chronic obstructive pulmonary disease, interstitial lung disease, or obstructive sleep apnea on CPAP therapy. Patients who have sleep apnea but are not heavily reliant on CPAP could also be counseled to refrain from using their CPAP mask for a few days. Alternatively, an internal jugular vein approach could be considered as it is less likely to result in iatrogenic pneumothorax. Additionally, the patient population at our facility mainly lives in rural areas, sometimes hours away from medical intervention. This case had a somewhat fortunate outcome considering what potentially could have happened to the patient.
Conclusion
Home CPAP use should be considered when making discharge decisions after procedures in the thoracic cavity. Even if the immediate postoperative CXR is negative, a large PTX can still develop if the patient is exposed to positive airway pressure. The mediastinal shift and/or rapid reversal of the shift can also dislodge pacemaker leads, so these devices need to be interrogated after treatment of their pneumothorax.
Lessons Learned
While some low-risk patients probably can be safely discharged shortly after pacemaker placement, there exists a subset of pacemaker patients, especially those who use nightly CPAP therapy, have chronic lung diseases, or live in rural areas, who will be best served with at least a night of observation to ensure that CPAP therapy does not lead to pneumothorax and lead dislodgement.
Authors
Van De Voort TJa; Burchill KJa,b
Author Affiliations
- Department of Surgery, University of North Dakota School of Medicine and Health Sciences, Grand Forks, ND 58203
- Department of Surgery, Veterans Affairs Medical Center, Fargo, ND 58102
Corresponding Author
Tyler J. Van De Voort, MD
1301 N. Columbia Road
RM E270, Stop 9037
Grand Forks, ND 58203
Email: tyler.vandevoort@ndus.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: December 10, 2020
Revision received: February 13, 2021
Accepted: March 4, 2021
References
- Rehaman A, Ramesh A, Prajapati S, Basavappa R. Lead displacement due to tension pneumothorax following permanent pacemaker implantation. J Cardiol Cases. 2016;15(1):25-27. Published 2016 Nov 17. doi:10.1016/j.jccase.2016.09.005
- Mao JT, Bernabei A, Cutrufello N, Kern JD. Spontaneous pneumothorax caused by excessive positive airway pressure therapy for obstructive sleep apnea. In: American Journal of Respiratory and Critical Care Medicine. American Thoracic Society International Conference Abstracts. American Thoracic Society; 2018:A6682.
- Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac Pacemakers: Function, Troubleshooting, and Management: Part 1 of a 2-Part Series. J Am Coll Cardiol. 2017;69(2):189-210. doi:10.1016/j.jacc.2016.10.061
- Tsotsolis N, Tsirgogianni K, Kioumis I, et al. Pneumothorax as a complication of central venous catheter insertion. Ann Transl Med. 2015;3(3):40. doi:10.3978/j.issn.2305-5839.2015.02.11
- Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331(26):1735-1738. doi:10.1056/NEJM199412293312602
- Langner S, Kolditz M, Kleymann J, et al. Großer Pneumothorax unter CPAP-Therapie beim Schlafapnoepatienten ohne vorbekannte Lungen- und Thoraxerkrankungen – ein Fallbericht [Large Pneumothorax in a Sleep Apnea Patient with CPAP without Previously Known Lung and Thoracic Diseases - a Case Report]. Pneumologie. 2020;74(4):217-221. doi:10.1055/a-1108-3004
- Hsu CW, Sun SF. Iatrogenic pneumothorax related to mechanical ventilation. World J Crit Care Med. 2014;3(1):8-14. Published 2014 Feb 4. doi:10.5492/wjccm.v3.i1.8
- Iyer HV. Pneumothorax in the ventilated patient: a difficult problem to recognize. J Am Coll Surg. 2010;210(6):1013. doi:10.1016/j.jamcollsurg.2010.01.024
- Ghani A, Delnoy PP, Ramdat Misier AR, et al. Incidence of lead dislodgement, malfunction and perforation during the first year following device implantation. Neth Heart J. 2014;22(6):286-291. doi:10.1007/s12471-014-0556-6