Figure 2. Gross specimen of pylorus-sparing pancreaticoduodenectomy with a mass in pancreatic head.
She tolerated the procedure well and was discharged home after seven days following an uncomplicated postoperative course. Final pathology confirmed the diagnosis of a noninvasive SPT with negative resection margins. The patient recovered without complication and will undergo surveillance imaging six months after surgery.
Discussion
Due to the rareness of pancreatic tumors in the pediatric population, there is a paucity of data on the topic. Most understanding of these tumors comes from case studies from large tertiary institutions, which pool data on all types of pediatric pancreatic masses. Our case features a previously healthy young girl who presented with severe abdominal pain, a profound systemic inflammatory response, and an inflammatory mass within the pancreatic head. While infectious etiologies were considered, FNA of the mass confirmed SPT of the pancreas.
SPTs account for approximately 2 to 3 percent of all pancreatic tumors, regardless of age.3 Though pancreatic neoplasms are exceedingly rare in children, SPTs are one of the most common histologies of such lesions, accounting for 8 to 44 percent.3 SPTs occur most commonly during the third decade of life, but up to 22 percent are noted to occur in individuals <19 years old.4 They disproportionately affect women at an overall ratio of 10:1, though this gender discrepancy is less prominent in children.3,5 With regards to pediatric patients, the three largest series of SPTs report a median age at presentation of 13–15 years.3,6,7 Though no series includes demographic information on pubertal status, it is reasonable to deduce that such a tumor is exceedingly rare in prepubertal patients such as ours.
This patient's presentation of abdominal pain and emesis is consistent with prior literature, which reports abdominal symptoms to be the most common presenting complaints (67–73 percent).3,7-9 Although our patient did not have a palpable mass on exam, some series indicate that children are more likely than adults to present with a palpable abdominal mass.10 Fever, which was present in our patient, is a fairly uncommon presenting symptom (4–17 percent).8,9 Further, our literature review suggests that our patient represents the first reported case of a SPT presenting as an inflammatory mass in a child.
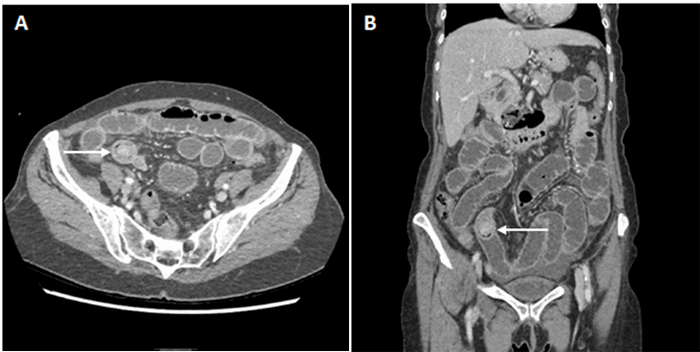
The etiology of our patient's mass was initially thought to be infectious given her clinical presentation, which ultimately provoked an ERCP with FNA to obtain a definitive diagnosis. However, imaging is frequently sufficient for diagnosis in many patients, making further preoperative workup unnecessary. Pediatric cases series have reported rates of preoperative FNA as low as 17 percent.6 Though the radiologic features of this tumor have been extensively described, findings may be elusive, and further diagnostics may be required.
PD is considered the mainstay of surgical treatment for tumors of the pancreatic head; however, it is rarely performed in children. Mortality and morbidity rates following PD in adult patients range from 1 to 3 percent and 30 to 40 percent, respectively.11,12 Similarly, morbidity rates following PD in children are high, ranging from 29 to 50 percent. Reported complications include intraabdominal abscess, pancreatic fistula, pancreatic leak, and chyle leak.9,11-14 Nevertheless, PD has proven to be safe for children in several series, including those as young as 3–4 years old, with SPT appearing to be one of the more common indications for such treatment.3,6-8,12-14 Our patient is one of the youngest reported to undergo PD for a pancreatic SPT and possibly the youngest to undergo PD for SPT in the United States. The postoperative course was uncomplicated, and she remains without issue after five months of follow-up.
Our patient underwent a pylorus-sparing PD, consistent with prior literature on this topic.9,13 Pylorus preservation remains critical when performing PD for pediatric patients given the desire to avoid hindering future growth and development. The outcome for patients with SPT is excellent, with 2- and 5-year survival estimated to be 97 percent and 95 percent, respectively.4 Overall, these tumors tend to be indolent, slow-growing, and have a low risk of malignant potential.3 Age under 13.5 years at diagnosis, tumor rupture and metastases have been identified as risk factors for recurrence.15 Surgical resection remains the mainstay of treatment and is indicated even in the presence of local invasion and metastatic disease.7
Conclusion
Complete resection with pylorus-preserving PD was performed in a young girl with SPT, and no complications occurred. Consistent with prior reports, PD appears to be a safe and curative option for pediatric patients with SPT of the pancreatic head. In addition, our case highlights the fact that, although rare, SPT should be considered a potential diagnosis for children presenting with a primary inflammatory mass of the pancreas. If the exact etiology remains unclear based on imaging, ERCP with FNA can help make the diagnosis and guide definitive treatment.
Lessons Learned
The presentation of solid pseudopapillary tumors is variable and rare in the pediatric population. That said, it is always most appropriate to expect the expected while searching for the unexpected in the case of a pediatric patient with the unusual presentation of a mass in the head of the pancreas. In general, the prognosis for these patients is generally very good, and pancreaticoduodenectomy is a safe and well-tolerated form of curative treatment.
Authors
Marina L Reppucci, MD
Department of General Surgery, Icahn School of Medicine at Mount Sinai, New York, NY
Joseph J Kim, MD
Department of Surgical Oncology, Icahn School of Medicine at Mount Sinai, New York, NY
Umut Sarpel, MD, FACS
Department of Surgical Oncology, Icahn School of Medicine at Mount Sinai, New York, NY
Brian A. Coakley, MD
Department of Pediatric Surgery, Icahn School of Medicine at Mount Sinai, New York, NY
Correspondence Author
Dr. Brian A. Coakley
Assistant Professor of Surgery, Pediatric Surgery
Icahn School of Medicine at Mount Sinai
One Gustave L. Levy Place, Box 1259, New York, NY, 10029
Phone: 212-241-1608
Email: brian.coakley@mountsinai.org
Disclosure Statement
The authors have no conflicts of interest to report.
References
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2011. In. Bethesda, MD: National Cancer Institute; November 2013.
- National Cancer Institute Surveillance E, and End Results (SEER) Program Public USe Date (1973-2005). National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program Public USe Date (1973-2005). National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, release April 2008, based on the November 2007 submission. Available at: www.seer.cancer.gov In.
- Speer AL, Barthel ER, Patel MM, Grikscheit TC. Solid pseudopapillary tumor of the pancreas: a single-institution 20-year series of pediatric patients. J Pediatr Surg. 2012;47(6):1217–1222.
- Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200(6):965–972.
- Antoniou EA, Damaskos C, Garmpis N, et al. Solid Pseudopapillary Tumor of the Pancreas: A Single-center Experience and Review of the Literature. In Vivo. 2017;31(4):501–510.
- Choi SH, Kim SM, Oh JT, Park JY, Seo JM, Lee SK. Solid pseudopapillary tumor of the pancreas: a multicenter study of 23 pediatric cases. J Pediatr Surg. 2006;41(12):1992–1995.
- Hwang J, Kim DY, Kim SC, Namgoong JM, Hong SM. Solid-pseudopapillary neoplasm of the pancreas in children: can we predict malignancy? J Pediatr Surg. 2014;49(12):1730–1733.
- van den Akker M, Angelini P, Taylor G, Chami R, Gerstle JT, Gupta A. Malignant pancreatic tumors in children: a single-institution series. J Pediatr Surg. 2012;47(4):681–687.
- Lindholm EB, Alkattan AK, Abramson SJ, et al. Pancreaticoduodenectomy for pediatric and adolescent pancreatic malignancy: A single-center retrospective analysis. J Pediatr Surg. 2017;52(2):299–303.
- Lee SE, Jang JY, Hwang DW, Park KW, Kim SW. Clinical features and outcome of solid pseudopapillary neoplasm: differences between adults and children. Arch Surg. 2008;143(12):1218–1221.
- Newhook TE, LaPar DJ, Lindberg JM, Bauer TW, Adams RB, Zaydfudim VM. Morbidity and mortality of pancreaticoduodenectomy for benign and premalignant pancreatic neoplasms. J Gastrointest Surg. 2015;19(6):1072–1077.
- Mansfield SA, Mahida JB, Dillhoff M, et al. Pancreaticoduodenectomy outcomes in the pediatric, adolescent, and young adult population. J Surg Res. 2016;204(1):232–236.
- d'Ambrosio G, del Prete L, Grimaldi C, et al. Pancreaticoduodenectomy for malignancies in children. J Pediatr Surg. 2014;49(4):534–538.
- Scandavini C, Valente R, Rangelova E, et al. Pancreatectomies for pancreatic neoplasms in pediatric and adolescent age: A single institution experience. Pancreatology. 2018;18(2):204–207.
- Irtan S, Galmiche-Rolland L, Elie C, et al. Recurrence of Solid Pseudopapillary Neoplasms of the Pancreas: Results of a Nationwide Study of Risk Factors and Treatment Modalities. Pediatr Blood Cancer. 2016;63(9):1515–1521.