Discussion
Soft tissue sarcomas (STS) are a heterogeneous group of neoplasms with mesenchymal origin. There are more than 100 histological subtypes of STS and can occur anywhere. The majority occur in the extremities (75 percent), most commonly the thigh. Around 10 percent are located each in the trunk wall and retroperitoneum.1,2 Accurate and prompt diagnosis of STS is frequently delayed due to its rarity in addition to patient and physician assumption of benign etiology.3 A soft tissue mass is 100 times more likely to be benign than malignant, a statistic that impacts the sensitivity for the detection of STS.1 Surgical excision is the primary treatment of STS with adjuvant or neo-adjuvant adjuncts employed as needed based on staging.2 Special consideration is paid to preservation of limb functionality in extremity sarcomas. The achievement of negative surgical margins is the most important variable in determining adequate local control.2 Positive margins are associated with increased risk of both local recurrence and distant metastasis.3 In addition, a prospective review of 365 patients revealed that tumor depth was the most sensitive marker of metastatic disease.4
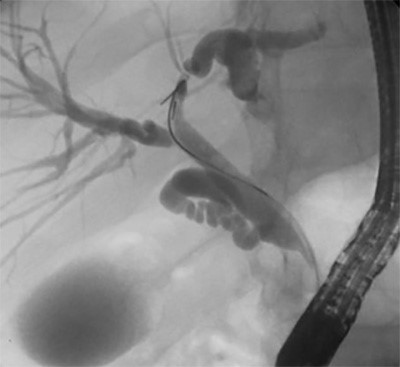
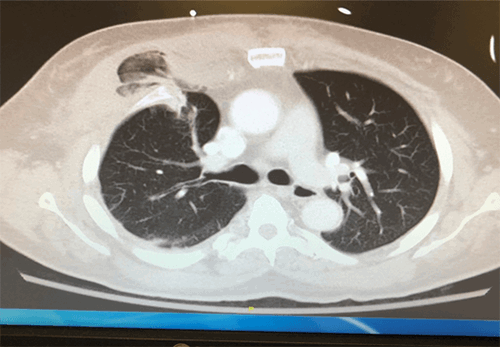
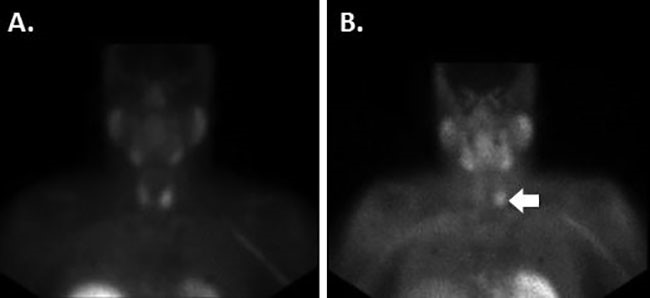
Our patient’s clinical course was complicated by the presence of a muscular tear leading to recurrent hematoma that obscured the identification of STS and delayed diagnosis for a significant period. The initial CT that was obtained on presentation was read as “unable to exclude a soft tissue sarcoma.” However, the patient’s history in conjunction with an outpatient MRI that was consistent with an intramuscular hematoma presumptively eliminated malignancy from our differential diagnosis. This ultimately had a negative impact on our patient’s outcome, as tissue biopsy should have been a paramount objective during initial operative management. Furthermore, it was likely that the margins of the mass were violated as a result of the multiple incision and drainage procedures that the patient underwent. This further complicated excision of the mass and subsequent analysis of anatomic pathology. However, once diagnosis of pleomorphic sarcoma was made, appropriate metastatic workup was initiated and remarkable for suspicious pelvic lymph nodes. Adequate steps were then made to refer the patient to appropriate oncological services and a more specialized multimodal treatment team.
Conclusion
Current literature recommends that patients with high suspicion of having an STS be referred to a specialized tertiary care center.1 Initial approach to a soft tissue lesion must include a thorough assessment for atypical features in clinical presentation. MRI is the most useful test for the initial diagnosis of a STS and should be utilized as the primary imaging modality.2 However, due to the low incidence of STS, a malignancy is unlikely to be incidentally identified. In our case, the delayed presentation of hematoma in a patient without anticoagulation therapy should have heightened our concern for underlying pathology.
Lessons Learned
Atypical presentations of benign processes with nonspecific CT findings should increase index of suspicion for STS. Referral to a dedicated tertiary center following proper evaluation with definitive diagnosis or inability to rule out the presence of STS is the primary step for plan of care. Recruitment of a specialized multimodal team should occur prior to surgical intervention.
Authors
Anna L. Shu, DO
St. Joseph Mercy Oakland
Department of General Surgery
Pontiac, MI
Joyce R. Iwema, MD
St. Joseph Mercy Oakland
Department of General Surgery
Pontiac, MI
Harrison S. Browning, BS
St. Joseph Mercy Oakland
Department of General Surgery
Pontiac, MI
Malik E. McKany, MD
St. Joseph Mercy Oakland
Department of General Surgery
Pontiac, MI
Correspondence
Anna Shu, DO
44405 Woodward Avenue
Pontiac, MI 48341
Phone: 248-227-7962
E-mail: alinshu@gmail.com
Meeting Presentations
St Joseph Mercy Regional Resident Research Day
Pontiac, MI
March 28, 2018
Disclosures
The authors have no conflicts of interest to disclose.
References
- Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F. World Health Organization Classification of tumours of soft tissue and bone, 4th, IARC Press, Lyon. 2013.
- ESMO/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014; 25 Suppl 3:iii102–112.
- Trovik CS, Bauer HC, Alvegård TA, et al. Surgical margins, local recurrence and metastasis in soft tissue sarcomas: 559 surgically-treated patients from the Scandinavian Sarcoma Group Register. Eur J Cancer. 2000; 36:710–716.
- Hussein R, Smith MA. Soft tissue sarcomas: are current referral guidelines sufficient? Ann R Coll Surg Engl. 2005; 87:171–173.