Figure 3. Chest X ray after placement of percutaneous drain.
Patient’s cardiovascular function improved following placement of the mediastinal drain, with subsequent imaging showing resolution of the pneumomediastinum. Patient’s hypotension resolved, and he was weaned off of vasopressor support. The mediastinal and left pleural drains were removed relatively early in the patient’s hospital course, which was prolonged by multiple infections secondary to the patient’s known HIV status. He was eventually discharged from the hospital to an extended care facility.
Discussion
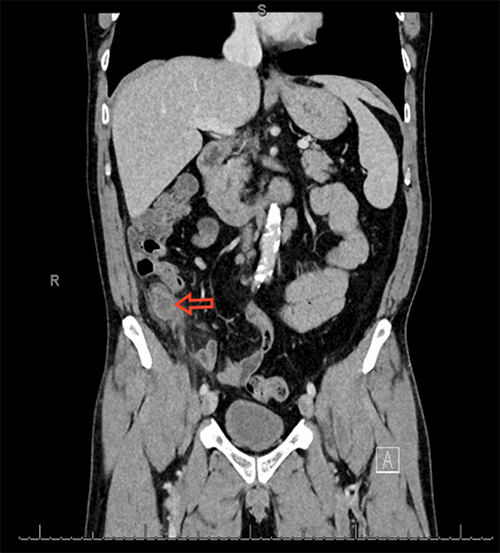
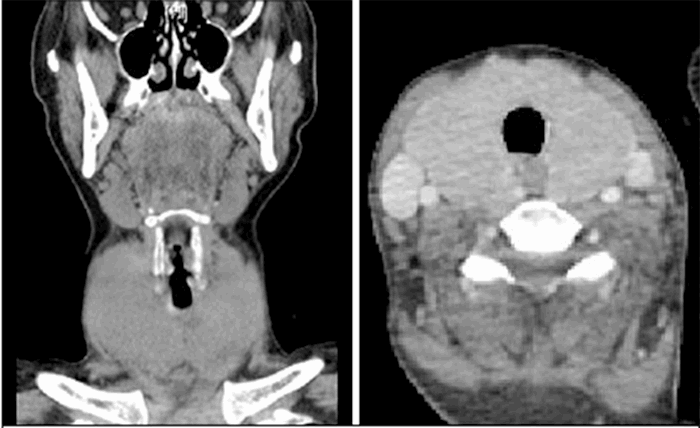
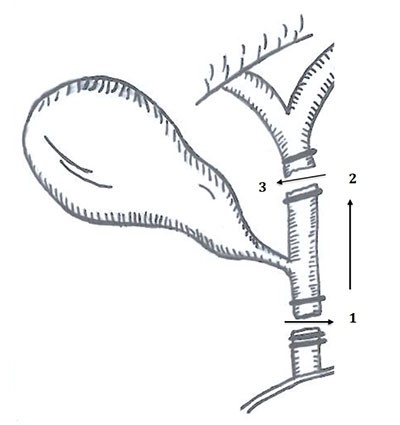
The phenomenon commonly referred to as pneumomediastinum consists of free air within the connective tissue of the mediastinum.1 Pneumomediastinum can be a consequence of either blunt or penetrating thoracic trauma. The development of tension pneumomediastinum can be associated with injury to the tracheobronchial tree or esophagus, both of which can be life-threatening if primary repair of the injury is not addressed. These injuries, however, are rare findings in patients who survive to be seen in the hospital. One single-center study examining incidence of pneumomediastinum found a mean age of 40, in predominantly male (69.8 percent) trauma patients.2 A large retrospective study found 5.2 percent (71/1364) of their trauma patients over an eight-year period had CT findings of pneumomediastinum. Of those patients, 5.8 percent (4/68) required surgical repair.3 The diagnosis of tension pneumopericardium can be seen on CT as a “flattened heart sign,” in which the anterior face of the heart is flattened, resulting in a decrease in the anterior-posterior diameter. The authors describing the flattened heart sign believe the sign to be diagnostic and predictive of a poor prognosis, though it may lead to early diagnosis and treatment.4 This sign is again demonstrated in Figure 2. We believe our approach to be a relatively novel technique involving the percutaneous placement of a central venous catheter, which was then placed to water seal using a standard underwater seal system. To our knowledge, only four other authors have attempted a percutaneous catheter placement for relief of tension pneumomediastinum:
- The first case involved the placement of a pericardiocentesis catheter as a stabilizing measure before conversion to a pericardial window in the operating room.5
- The second case involved placement of a pigtail catheter via a subxiphoid approach; however, significant additional details were not provided.6
- In the third case, the catheter was attached to a Heimlich valve and the catheter was removed and re-inserted multiple times during the patient’s hospital course.7
- The final case used needle decompression of the pericardium to stabilize the patient. Following stabilization, an 18 French triple-lumen catheter was placed, through which air could be aspirated as needed.8
In comparison with these cases, our catheter was placed to an underwater seal system, where it remained until resolution of the tension pneumomediastinum.
Conclusion
Tension pneumomediastinum is a rare, life-threatening sequela of torso trauma that necessitates urgent intervention. Prompt recognition and relief of tension physiology is the priority. Decompression of the mediastinum can be accomplished using a variety of techniques. After initial decompression, the patient needs to be evaluated for the source of the air, as further intervention to repair an aerodigestive injury may be necessary.
Lessons Learned
We believe our approach to be a relatively novel technique involving the percutaneous placement of a central venous catheter, which was then placed to water seal using a standard underwater seal system. To our knowledge, only four other authors have attempted a percutaneous catheter placement for relief of tension pneumomediastinum.
Authors
Zachary A Spigel, MDa; Mohammed J Al Fayyadh, MBChB, MSCI-TSb; and Daniel L Dent, MD, FACSb
Correspondence Author
Dr. Zachary A Spigel
Allegheny Health Network
General Surgery Residency
320 E North Ave
Pittsburgh, PA 15212
210-274-4002
Zachary.Spigel@ahn.org
Author Affiliations
a Allegheny Health Network Medical Education Consortium, Department of Surgery, Pittsburgh, PA 15212
b University of Texas Health Science Center — San Antonio, Department of Surgery, San Antonio, TX 78229
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Demetriades D, Levy R, Hatzitheofilou C, Chun R. Tension pneumopericardium following penetrating trauma: case report. J Traum. Feb. 1990;30(2):238-9.
- Rezende-Neto JB, Hoffmann J, Al Mahroos M, et al. Occult pneumomediastinum in blunt chest trauma: clinical significance. Injury. Jan 2010;41(1):40-3.
- MacLeod J, Tibbs BM, Freiberger DJ, Rozycki GS, Lewis F, Feliciano DV. Pneumomediastinum in the injured patient: inconsequential or predictive? Am Surgeon. May 2009;75(5):375-7.
- Hernandez-Luyando L, Calvo J, de las Heras EG, De la Puente H, Lopez C. Tension pericardial collections: sign of ‘flattened heart’ in CT. Eur J Radiol. Nov 1996;23(3):250-2.
- Clouse WD, Dent DL, Stewart RM, Gray GA. Tension pneumopericardium from blunt chest trauma. Contemp Surg. 2003;59(6):271-5.
- Yadav S, Sadasivan D, Sharma S. Tension pneumopericardium relieved by pigtail catheter. Eur J Cardio-thorac. Feb 2005:344-344.
- Mohamed IS, Lee YH, Yamout SZ, Fakir S, Reynolds AM. Ultrasound guided percutaneous relief of tension pneumomediastinum in a 1-day-old newborn. Arch Dis Child-Fetal. Nov 2007;92(6):F458-458.
- Markarian MK, MacIntyre DA, Cousins BJ, Malone A, Fildes JJ. Adolescent pneumopericardium and pneumomediastinum after motor vehicle crash and ejection. Am J Emerg Med. May 2008;26(4):515-e1.