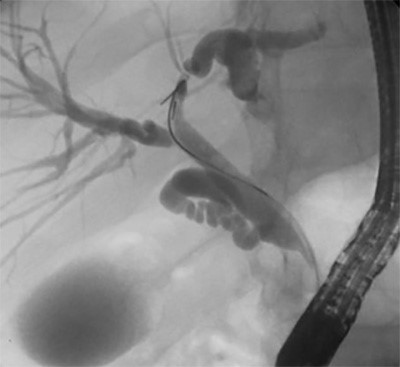
Figure 2: Intraoperative image of the internal jugular vein laceration after proximal and distal control of the vessel have been achieved.
The sternocleidomastoid muscle was then further mobilized medially to allow for a vessel loop to be passed around the proximal and distal extent of the vein for control of the vessel. The common facial vein was ligated using 3-0 silk sutures for better mobilization. Due to the longitudinal nature of the laceration, the internal jugular vein was primarily repaired with 5-0 Prolene sutures. Mild narrowing of the vein was noted; however, intraoperative ultrasonography revealed normal flow proximal and distal to the site of repair. Exploration of the carotid sheath, trachea and esophagus were unremarkable for additional injuries. The sternocleidomastoid muscle and the skin were primarily reapproximated, and the patient was extubated within the operating room and was found to have a normal neurologic exam.
On postoperative day one, a follow-up Doppler ultrasound revealed a nearly occlusive acute thrombus in the proximal internal jugular vein with distention of the vein above the thrombus. The external jugular and right innominate veins were patent with normal flow. The common carotid, internal carotid, and external carotid arteries were widely patent without thrombus. Low-dose aspirin was initiated (81 mg tablet daily for one month). At that time, the patient was tolerating a regular diet and ambulating independently without changes in his neurological status; he was hence discharged on postoperative day one with instructions to avoid contact sports for one month. On outpatient follow-up, the neck wound looked completely healed. No further imaging study was performed to assess for change in the IJV thrombus; however, the patient continued to remain asymptomatic.
Discussion
We report the management of an ice hockey skate blade laceration with an isolated IJV injury. Lacerations to the neck from ice skates are extremely rare, and the management of such life-threatening injuries is extraordinary sparse in the literature. Rasanen et al. reported the only three cases in the literature of detailed ice skate blade lacerations and their further management.1 One case in that series involved an IJV laceration that was identified and primarily repaired, and the remaining two cases involved trauma to the airway and other major neck vasculature that resulted in on-scene death prior to any intervention. We report and demonstrate the successful management of such an injury.
Previous, graphic accounts of televised National Hockey League (NHL) ice skate lacerations to the neck include Clint Malarchuk in 1989 and Richard Zednik in 2008.2 Malarchuk, an ice hockey goaltender for the Buffalo Sabres, was struck in the neck by an opposing team member’s skate blade, and his IJV was severed. More recently, Richard Zednik had a skate blade laceration injury to his right carotid artery. In both cases, the vessel injuries were primarily repaired and both athletes made complete recoveries without any neurovascular sequelae.
Hockey players are at risk for neck injuries when skate blades become airborne or in a position of movement that allows for contact with the neck of another player. Hockey is an environment that is prone to injury, given the combination of sharp blades, high skating velocities (up to 30 mph), and the aggressive, full-contact nature of the sport (body checking). Preventive measures can be taken to lessen the risk of neck injuries: a neck guard, which is protective equipment worn around the neck, acts as a barrier that absorbs the impact of external objects and helps deflect external forces as they come in contact with vital structures of the neck, minimizing the risk of severe injury.3 These guards consist of protective layers of Kevlar or Spectra-Guard. Most neck guards can withstand forces of 300 N (with some guards protecting against forces as high as 600 N).3 However, despite the utilization of protective equipment, both blunt and penetrating injuries have been reported in players wearing neck guards.
Managing penetrating neck injuries is based on the specific neck zone that has been injured. The neck is characteristically divided into three anatomic zones by the cricoid cartilage and mandible. Structures present between these two anatomical points fall within zone II of the neck and include major blood vessels, nerves, trachea, and esophagus, all of which are at risk of being injured. With advancements in diagnostic imaging and endoscopic technology, there has been a large shift from mandatory to selective neck exploration in penetrating neck trauma. The Western Trauma Association has created an algorithm for managing penetrating neck trauma that violate the platysma. This algorithm recommends surgical exploration if hard signs of major vascular or aerodigestive trauma are present, including airway compromise, subcutaneous emphysema, expanding hematoma, active bleeding, shock, neurologic deficit, or hematemesis.4 In the present case, the young athlete demonstrated active bleeding that warranted immediate surgical exploration. However, in asymptomatic patients without any signs of injury, a selective approach can be considered with computed tomography angiography (CTA) with or without esophagogastroduodenoscopy (EGD) and bronchoscopy if the patient is stable and able to tolerate such imaging modalities.5
Exploration of zone II should be most optimally accessed via a longitudinal incision anterior to the sternocleidomastoid muscle to maximize exposure. Once proximal and distal vascular control have been achieved, the surgeon can systematically explore remaining venous, arterial, and nervous structures as well as the trachea and esophagus in a systematic fashion. Consideration of either ligation or primary repair of the lacerated IJV is acceptable and should be based on the surgeon’s ability to control active hemorrhage, the patient’s hemodynamic status, and other potential injuries that may require additional care. Ligation should be strongly considered if the laceration disrupts a significant portion of the circumference of the IJV, or if a transection/uneven luminal injury is present that does not allow for an adequate repair. Currently, no data exists comparing the efficacy of either approach; however, the IJV can be ligated with minimal morbidity if required.6 Complications of IJV ligation are rare and most commonly include thrombosis.6
In the present case, postoperative Doppler assessment demonstrated a thrombosis at the laceration repair site; this was managed conservatively with antiplatelet therapy alone. However, in the setting of symptomatic IJV thrombosis, where clinical manifestation may include pain, cervical/arm edema, superficial varicose collateral veins, and indurated vein, anticoagulation should be considered for three to six months. Currently, no data suggests a more effective approach (no anticoagulation versus three to six months of anticoagulation) for asymptomatic IJV thrombosis. Prognosis and management should be individualized to the patient’s extent of deep venous thrombosis, if developed. Likewise, given the rarity of such injuries, there are no reports that detail the duration to return to full physical activity. In our case, the young athlete was instructed to avoid physical activity for up to four weeks. However, this should be individualized to each patient’s circumstance and be lengthened if greater severity or additional injuries exist.
Conclusion
Hockey players are at risk for penetrating neck injuries. A laceration to the internal jugular vein in the prehospital setting should be managed with a pressure dressing to tamponade bleeding and plans for immediate transfer to the appropriate hospital setting. If hard signs of vascular injury are present, then surgical exploration is warranted. Once the extent of the injury is visualized, primary repair with a 4-0 or 5-0 non-absorbable suture may be attempted. If repair cannot be performed, the IJV can be ligated with minimal morbidity.
Lessons Learned
Lacerations to zone II of the neck with hard signs of vascular injury may present with a profound amount of blood loss. Such injuries should be emergently explored in the appropriate surgical setting to achieve bleeding control. Appropriate management of an IJV laceration may include primary repair or vessel ligation and should be individualized to each case.
Authors
Asad J. Choudhry, MBBS
Department of Surgery, Mayo Clinic, Rochester, MN
Mohamed D. Ray-Zack, MBBS
Department of Surgery, Mayo Clinic, Rochester, MN
Moustafa Younis, MBBS
Department of Surgery, Mayo Clinic, Rochester, MN
Ramoncito David, MD
Department of Vascular Surgery, Mayo Clinic, Rochester, MN
Matthew C. Hernandez, MD
Department of Surgery, Mayo Clinic, Rochester, MN
Johnathon M. Aho, PhD
Department of Surgery, Mayo Clinic, Rochester, MN
Martin D. Zielinski, MD
Department of Surgery, Mayo Clinic, Rochester, MN
Correspondence Author
Dr. Martin D. Zielinski
Division of Trauma, Critical Care, and General Surgery
Mayo Clinic
200 First St SW
Rochester, MN 55905
507-255-2923
zielinski.martin@mayo.edu
Meeting Presentation
Presented at the joint Midwest and Central Surgical Association Meeting, July 31–August 1, 2017, in Chicago, Illinois.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Vergis A, Rasanen T, Hernefalk L. Neck injuries from skate blades in ice hockey: a report of three cases. Scand J Med Sci Sports. 1996;6(6):352–354.
- Malarchuk C. Bleeding Out. The Players' Tribune. 2018. https://www.theplayerstribune.com/en-us/articles/clint-malarchuk-bleeding-out. Published March 22, 2018. Accessed December 6, 2018.
- Loyd AM, Berglund L, Twardowski CP, et al. The most cut-resistant neck guard for preventing lacerations to the neck. Clin J Sport Med. 2015;25(3):254–259.
- Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg. 2013;75(6):936–940.
- Prichayudh S, Choadrachata-anun J, Sriussadaporn S, et al. Selective management of penetrating neck injuries using "no zone" approach. Injury. 2015;46(9):1720–1725.
- Gbaguidi X, Janvresse A, Benichou J, Cailleux N, Levesque H, Marie I. Internal jugular vein thrombosis: outcome and risk factors. QJM. 2011;104(3):209–219.