Figure 1. Axial CT images showing the presence of a hiatal hernia
a) Portion of large colon entering the hernia defect posterior to the esophagus
b) Decompressed colon distal to the colonic obstruction
c) Stomach and spleen within the abdomen near the defect
The patient was admitted and underwent intravenous fluid resuscitation. Because she had no emesis, no evidence of complete obstruction, and a competent ileocecal valve, no nasogastric tube was placed. Given the mechanical obstruction seen on imaging, our surgical team discussed the options for conservative or operative management with the patient. Conservative management was discussed, including nasogastric tube (NGT) decompression, continued intravenous fluids, daily laboratory markers, and serial abdominal exams. Consideration was given both to the fact that this treatment modality may fail as well as to the risks of organ ischemia if progression occurred. Given both the patient’s sleeve gastrectomy and current hiatal hernia, we also informed her that NGT placement might be difficult. The patient felt that surgical treatment with reduction of the colon and correction of the hernia defect was her best option for definitive resolution of her symptoms.
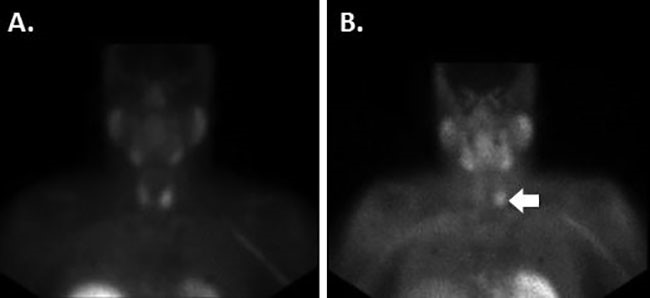
The patient was taken to the operating room the next day for laparoscopic hiatal hernia repair. Both the stomach and transverse colon were gently reduced back into the abdominal cavity using blunt bowel graspers. Due to the patient’s, prior sleeve gastrectomy, some peri-hiatal scar tissue was present that required lysis to aid in the full reduction of the stomach. A posterior cruroplasty was performed with non-permanent mesh reinforcement. A fundoplication was not performed because of her prior sleeve gastrectomy. Fluoroscopy obtained on postoperative day number one showed patency of the proximal upper gastrointestinal tract. The patient was immediately started on a general diet postoperatively and was able to be discharged home on the evening of postoperative day number two.
Discussion
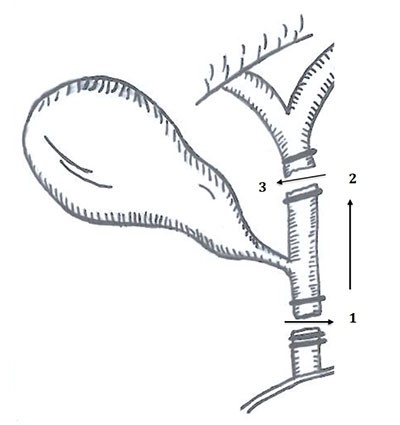
The four types of paraesophageal hernias are migration of the gastroesophageal (GE) junction above the esophageal hiatus (type 1), herniation of a portion of the stomach without movement of the GE junction (type 2), herniation of both the GE junction and a portion of the stomach (type 3), and herniation of both the stomach and other abdominal organs (type 4).1 Type 4 hernias most commonly contain the transverse colon, followed by the spleen, small bowel, large bowel, and pancreas.2,3 While there are several case reports of colonic obstruction due to hiatal hernia, there are none describing this condition after undergoing bariatric surgery.4-9
Sleeve gastrectomy is currently the most commonly performed procedure for morbid obesity.10 Postoperative complications include staple line leak, abscess formation, bleeding, trocar site herniation, bowel obstruction secondary to adhesive disease, and, according to more recent reports, hiatal hernia formation.11,12 The incidence of hiatal hernia in morbidly obese patients undergoing bariatric surgery is reported to be as high as 40 percent; if found during preoperative evaluation or intraoperatively, concomitant repair should be performed.13,14 Several cases of both acute and delayed hiatal hernia formation after either sleeve gastrectomy or Roux-en-Y gastric bypass have been reported in the literature, but none containing the large colon.15,16
It is imperative that physicians hold a suspicion for hiatal hernias in patients after bariatric surgery as a source of both gastric and bowel obstruction.8 A diagnosis can be made swiftly radiographically with barium study or computed tomography.1 Repair can be performed either laparoscopically or open and follows standard hiatal hernia repair. Surgical correction includes reduction of the contents of the hernia sac back into the abdominal cavity, hernia sac resection, approximation of the diaphragmatic crus with or without mesh reinforcement, and gastropexy.3 Performing a fundoplication after bariatric surgery is not technically feasible because of the lack of redundant gastric tissue due to prior sleeve gastrectomy. Mesh reinforcement is proven to have a lower incidence of recurrence than primary repair. Although there is no difference in complication rates between synthetic or biologic mesh, synthetic mesh proves to have a lower recurrence rate compared to that of biologic mesh.17
Conclusion
Hiatal hernias after sleeve gastrectomy are uncommon, but should be included in the differential diagnosis of a patient presenting with obstructive symptoms after surgery for morbid obesity. If diagnosed, urgent surgical exploration is required for reduction of the hernia contents to ensure that no sequela of obstruction occurs. While standard hiatal hernia repair can be safely achieved, an anti-reflux procedure is omitted due to limited stomach volume to create a fundoplication.
Lessons Learned
When hiatal hernias are seen preoperatively or intraoperatively for bariatric surgery, surgical correction should ideally be performed with mesh reinforcement to prevent further clinical progression. Because transverse colon can frequently be involved in type 4 hiatal hernias, a high suspicion must be kept for the possibility of obstruction after sleeve gastrectomy for such pathology.
Authors
Chandler S Cortina, MDa; Shauna M Sheppard, MDa; and Steven R Bonomo, MD, FACSb
Corresponding Author
Chandler S Cortina, MD
Rush University Medical Center, Department of Surgery
1653 West Congress Parkway, Suite 792
Chicago, IL, USA 60612
Phone Number (cell): 337-580-5926
Fax Number: 312-942-2867
E-mail: CSCortinaMD@gmail.com
Author Affiliations
a Rush University Medical Center and John H Stroger Hospital of Cook County Integrated General Surgery Residency Program, Chicago, IL, USA
b Associate Professor of Surgery, Department of Surgery, John H Stroger Hospital of Cook County, Chicago, IL, USA
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Kahrilas PJ, Kim HC, Pandolfino J. Approaches to the Diagnosis and Grading of Hiatal Hernia. Best Pract Res Clin Gastroenterol. 2008;22(4):601-616.
- Wichterman K, Geha AS, Cahow CE, Baue AE. Giant paraesophageal hiatus hernia with intrathoracic stomach and colon: the case for early repair. Surg. 1979;86(September (3)):497-506.
- Townsend CM, Beauchamp RD, Evers BM. "Chapter 42. Gastroesophageal Reflux Disease and Hiatal Hernia." Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 20th ed.; Saunders Elsevier, 2008.
- Janzing H, Meeuws R, Culignez F, Vermassen F. Recurrent sub-obstruction due to intermittent hiatal hernia of the transverse colon with intrathoracic stomach torsion. Acta Chir Belg. 1989;89(6):329-332.
- Tabira Y, Yoshida Y, Sakaguchi T, Yoshimatsu S. Isolated colonic hernia through the esophageal hiatus. Dis Esophagus. 2005;18(4):283-286.
- Drescher D, Gockel I, Helmreich-Becker I, Lang H. Giant paraesophgael herniation with intermittment prolapse into the thorax of the transverse colon. Dtsch Med Wochenschr. 2011;136(5):213-216.
- Clark AJ, Madiba TE. Sliding hiatal hernia with intrathoracic stomach and obstructed colon. SAJS. 2002;40(3):101-102.
- Felsher J, Brodsky J, Brody F. Isolated Trans-hiatal Colonic Herniation. J Laparoendosc Adv Surg Tech A. 2003;13(2):105-108.
- Farrell B, Gerard PS, Bryk D. Paraesophageal hernia causing colonic obstruction. J Clin Gastroenterol. 1991;13:188-190.
- Reames FB, Finks FJ, Bacal D, et al. Changes in bariatric surgery procedure use in Michigan 2006-2013. JAMA. 2014;9:959-961.
- Gumbs AA, Gagner M, Dakin D, et al. Sleeve gastrectomy for morbid obesity. J Obes Surg. 2007;17:962-969.
- Márquez MF, Ayza MF, Lozano RB, et al. Gastric leak after laparoscopic sleeve gastrectomy. J Obes Surg. 2010;20:306-1311.
- Che F, Nguyen B, Cohen A, Nguyen NT. Prevalence of hiatal hernia in the morbidly obese. Surg Obes Relat Dis. 2014;9(6):920-924.
- Pham DV, Protyniak B, Binenbaum SJ, Squillaro A, Borao FJ. Simultaneous laparoscopic paraesophageal hernia repair and sleeve gastrectomy in the morbidly obese. Surg Obes Relat Dis. 2014;10(2):257-261.
- Al-Sanea O, Al-garzaie A, Dernaika M, Haddad J. Rare complication post sleeve gastrectomy: Acute irreducible paraesophageal hernia. Int J Surg Case Rep. 2015;8:88-91.
- Iannelli A, Kassir R, Schneck AS, Martini F, Gugenheim J. Hiatal hernia of the Roux-en-Y gastric bypass pouch 8 years after surgery. J Obes Surg. 2014;9:1494-1496.
- Huddy JR, Markar Sr, Ni MA, et al. Laparoscopic repair of hiatus hernia: Does mesh type influence outcome? A meta-analysis and European survey study. Surg Endosc. 2016;30(12):5209-5221.