Attempts to retrieve the coils endoscopically were unsuccessful given their small, mobile nature. Direct visualization of the bowel lumen confirmed absence of obstruction. Examination of the jejuno-jejunal anastomosis and the Roux limb were normal. Patient was maintained on total parenteral nutrition until an upper gastrointestinal contrast study on post-procedure day seven demonstrated no leak. She was then started on low-volume enteral feedings, which were advanced to her goal rate without complication. The coils were not visualized on further imaging and no additional endoscopy was performed. Patient continues to have routine follow-up with the surgery clinic, has had the drains removed, and is currently in stable condition one year later.
Discussion
This case demonstrates an uncommon series of complications secondary to initial CBD injury during an elective cholecystectomy. HAP secondary to iatrogenic injury continues to be exceedingly rare with only five reported cases in the last 24 years.2 Endovascular therapies have evolved into the first line treatment for the management visceral pseudoaneurysms. Compared to open surgery, there is reduced morbidity and mortality with similar survival rates long term.3 However, there are limited reports illustrating patient complications post-coil embolization of visceral vasculature. Current literature suggests they are rare, but may include delayed hemorrhage, infarction, necrosis, abscess formation, bilioma or biliary fistula.4
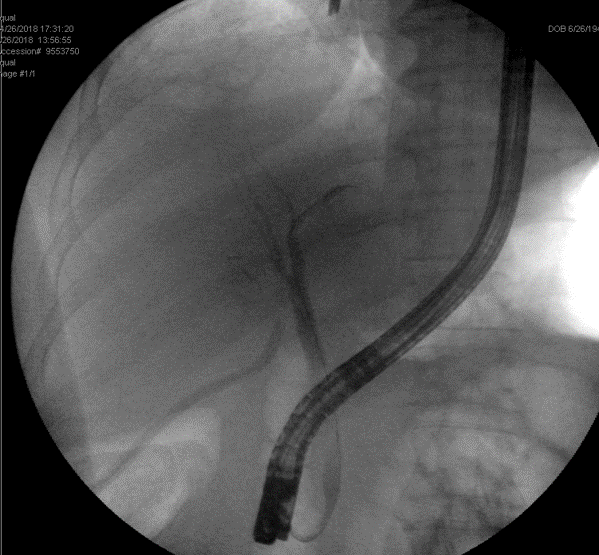
Multiple embolization strategies for treating visceral artery pseudoaneurysms exist that derive from a concept of occluding blood flow into the sac to prevent expansion and rupture. Available methods include coiling of the sac, deployment of covered stent grafts across the sac, coiling through a bare stent, liquid embolic agents, and thrombin injections for more superficially located target sites.3 In the setting of HAP, the injury is more common in the extrahepatic segment of the proximal hepatic artery, and endovascular stent-grafting should be considered as first line therapy.5-6 Covered stent grafts are of benefit as they are designed to inhibit sac inflow while maintaining parent vessel patency. However, vessel size, tortuosity and inadequate landing zones may preclude stent-grafting. Coiling of the pseudoaneurysm sac was the chosen intervention for this patient. When packed into a pseudoaneurysm, coils occlude arterial inflow and induce inflammation and thrombosis through their thrombogenic fibers.7 Coiling is indicated for pseudoaneurysms with short necks as those with wide necks have an increased risk for non-target embolization. Parent artery embolization is another option, however there is a risk of end-organ ischemia in the absence of collateral perfusion.7
Prior to any intervention, patients require imaging assessment with computed tomography angiogram (CTA) or magnetic resonance angiogram (MRA) to better understand vascular anatomy. Postoperatively, patients require a repeat angiogram or Duplex ultrasound to ensure successful occlusion with lack of pseudoaneurysm inflow. Postembolization syndrome may develop one to three days following intervention and will present as fever, nausea, and malaise with leukocytosis. The management of this syndrome is focused on alleviation of symptoms with antipyretics, antiemetics, and analgesics. Other complications include non-target embolization, abscess formation, and end-organ ischemia. Ultimately, patients should have routine follow-up in interventional radiology outpatient clinic with CTA or MRA at one month, six months, and then yearly to assess pseudoaneurysm sac size and adequate end organ perfusion.
As innovations continue to drive endovascular interventions, it is important to share experiences of rare complications for the purposes of optimizing clinical skill, safety, and the quality of care delivered to patients. This case provides a unique learning opportunity to highlight a rare complication of coil embolization in the context of a complex surgical patient who underwent the most common procedure performed by general surgeons. In this particular patient, her vascular anatomy was not suitable for stent grafting. The erosion of the coils into the small bowel may have been from either coil pack expansion or exacerbation of what was originally an unknown mycotic pseudoaneurysm. Proximal and distal embolization may have avoided this complication and is ultimately what was required. Endovascular interventions have promising outcomes and reduced morbidity for cases such as this one. However, it is imperative surgeons are aware of the types of interventions available, the indications for each and the potential complications following such procedures.
Conclusion
This case provides insight into technical considerations when coiling visceral pseudoaneurysms, as well as diagnosing and managing a novel complication, an arterio-enteric fistula secondary to coil erosion into the proximal small bowel. The treatment of this patient’s complications required multiple procedures from a multidisciplinary team, including surgery, interventional radiology, and gastroenterology. To our knowledge, such a complication has not been reported in the literature. We hope sharing this experience has the potential to improve the quality of care provided to our patients.
Lessons Learned
Endovascular stent-grafting should be considered first line in extrahepatic arterial pseudoaneurysms. Pseudoaneurysm sac embolization in such cases has a risk for coil erosion and migration.
Authors
Abhishek Jairama
UC Davis School of Medicine
Departments of Surgery and Radiology
Sacramento, CA
Alicia Gingrich, MD
UC Davis School of Medicine
Departments of Surgery and Radiology
Sacramento, CA
Catherine Vu, MD
UC Davis School of Medicine
Departments of Surgery and Radiology
Sacramento, CA
Brian C. Beldowicz, MD
UC Davis School of Medicine
Departments of Surgery and Radiology
Sacramento, CA
Uniformed Services University of the Health Sciences
Department of Military and Emergency Medicine
Bethesda, MD
Correspondence
Abhishek Jairam
UC Davis School of Medicine
4610 X Street. Sacramento, CA 95817
Phone: 805-796-7299
E-mail: akjairam92@gmail.com
Disclosures
The authors have no conflicts of interest to disclose.
References
- Raashed S, Chandrasegaram MD, Alsaleh K, et al. Vascular coil erosion into hepaticojejunostomy following hepatic arterial embolisation. BMC Surg. 2015;(15):51.
- Pulitanó C, Parks RW, Ireland H, et al. Impact of concomitant arterial injury on the outcome of laparoscopic bile duct injury. Am J Surg 2011;201(2):238–244.
- Saad NE, Saad WE, Davies MG, et al. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25:73–89
- Moukaddam H, Al-Kutoubi A. Pseudoaneurysms of hepatic artery branches: treatment with self-expanding stent-grafts in two cases. J Vasc Interv Radiol. 2007;18(7):897–901.
- Laganà D, Carrafiello G, Mangini M, et al. Multimodal approach to endovascular treatment of visceral artery aneurysms and pseudoaneurysms. Eur J Radiol. 2006;59(1):104–11.
- Berceli SA. Hepatic and splenic artery aneurysms. Semin Vasc Surg. 2005;18(4):196–201.
- Madhusudhan KS, Venkatesh HA, Gamanagatt S, et al. Interventional radiology in the management of visceral artery pseudoaneurysms: a review of techniques and embolic materials. Korean J Radiol. 2016;17(3):351–363.