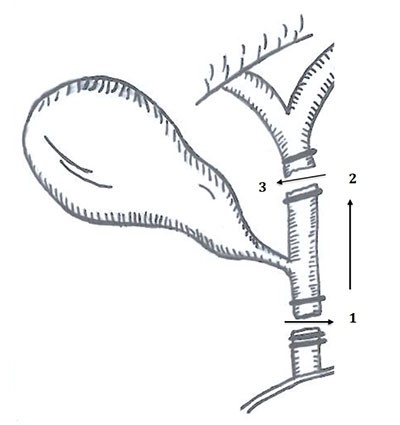
Figure 5. Primary GSF Cases
Endo=endoscopy, CT=computed tomography, Cysto=cystography, abd=abdomen, PET=positron emission tomography, A/P=abdomen and pelvis, LUQP=left upper quadrant pain, const. sx=constitutional symptoms, LAD=lymphadenopathy, WL=weight loss, SOB=shortness of breath, DOE=dyspnea on exertion, chemo=chemotherapy, p.gast.=partial gastrectomy, splen.=splenectomy, d. panc.=distal pancreatectomy, RT=radiation therapy, LND=lymph node dissection, t. gast.=total gastrectomy, Dz=disease, yr=year, mo=month, w/o=without, f/u=follow-up, DLBCL= Diffuse Large B Cell Lymphoma, PSL= Primary Splenic Lymphoma, PGL=Primary Gastric Lymphoma
With a paucity of data on individual chemotherapy regimens in the cases found, it is difficult to find even a correlative link between a particular chemotherapy agent or regimen and GSF formation. Our patient had recently received ibrutinib, which was shortly after discontinued due to toxicity (three months prior to presentation). Again, it is difficult to draw any correlation between this and GSF formation.
Chemotherapy as stand-alone management of GSF without resection was employed in three cases. Two cases21,24 cited the reason for nonoperative management as the patients’ poor health and high perioperative risk; the last case did not specify.12 One case reported disease free survival at publication less than a year later.21 Of the other two, one was lost to follow-up, and the second died at two months after diagnosis.12,24 Additionally, a single nonoperatively managed GSF case secondary to mucosal associated lymphoid tissue (MALT) lymphoma was treated solely with Helicobacter pylori triple therapy after the patient declined resection; there was no reported follow-up.8
Conclusion
Gastrosplenic fistulas are rare events that nearly always occur in the setting of lymphoma, and nearly always with DLBCL. They arise either in the setting of primary tumor necrosis or secondary to chemotherapy induced necrosis that has breached the splenic capsule.
This is the most comprehensive collection of GSF cases collected to date. Our case illustrates the high degree of suspicion that must be exercised in this patient population, as our patient presented with uncommon symptoms of GSF. Known splenic masses in the context of lymphoma should undergo follow-up and serial imaging to monitor for radiographic evidence of complications such as GSF.
Surgical resection with or without adjuvant chemotherapy is the definitive management of GSF if the patient can tolerate an operation due to the risk for hemorrhage described above. Poor surgical candidates can undergo chemotherapy as stand-alone treatment.
Lessons Learned
Gastrosplenic fistulas secondary to lymphoma occur after tumor necrosis either primarily or from chemotherapy. Surgical resection with or without adjuvant chemotherapy is the definitive management of GSF if the patient can tolerate an operation.
Authors
Slagle DLa, Jorge JMb, Nagle Ab
Correspondence Author
Alexander P. Nagle, MD, FACS
Northwestern University Department of Surgery
676 N. St. Clair St., Suite 650
Chicago, IL 60611
312-695-0641
a-nagle@northwestern.edu
Author Affiliations
- Feinberg School of Medicine, Northwestern Memorial Hospital, Chicago, IL
- Department of General Surgery, Northwestern Memorial Hospital, Chicago, IL
References
- Aribaş BK, Başkan E, Altinyollar H, Ungül U, Cengiz A, Erdil HF. . Gastrosplenic fistula due to splenic large cell lymphoma diagnosed by percutaneous drainage before surgical treatment. Turk J Gastroenterol 2008;19(1): 69-70.
- Bubenik O, Lopez MJ, Greco AO, Kraybill WG, Cherwitz DL. . Gastrosplenic fistula following successful chemotherapy for disseminated histiocytic lymphoma. Cancer 1983;52(6): 994-996.
- Gentilli S, Oldani A, Zanni M. . Gastro-splenic fistula as a complication of chemotherapy for large B cell lymphoma. Ann Ital Chir 2016;87.
- Hiltunen KM, Airo I, Mattila J, Helve O. . Massively bleeding gastrosplenic fistula following cytostatic chemotherapy of a malignant lymphoma. J Clin Gastroenterol 1991;13(4): 478-481.
- Moghazy KM. Gastrosplenic fistula following chemotherapy for lymphoma. Gulf J Oncolog 2008;(3): 64-67.
- Palmowski M, Zechmann C, Satzl S, Bartling S, Hallscheidt P. Large gastrosplenic fistula after effective treatment of abdominal diffuse large-B-cell lymphoma. Ann Hematol 2008;87(4): 337-338.
- Seib CD, Rocha FG, Hwang DG, Shoji BT. Gastrosplenic fistula from Hodgkin's lymphoma. J Clin Oncol 2009;27(20): e15-17.
- Senapati J, Devasia AJ, Sudhakar S, Viswabandya A. Asymptomatic gastrosplenic fistula in a patient with marginal zonal lymphoma transformed to diffuse large B cell lymphoma—a case report and review of literature. AnnHematol 2014;93(9): 1599-1602.
- Sousa M, Gomes A, Pignatelli N, Nunes V. Massive gastrointestinal bleeding after chemotherapy for gastric lymphoma. Int J Surg Case Rep 2016;21: 41-43.
- Al-Ashgar HI, Khan MQ, Ghamdi AM, Bamehriz FY, Maghfoor I. Gastrosplenic fistula in Hodgkin's lymphoma treated successfully by laparoscopic surgery and chemotherapy. Saudi Med J 2007;28(12): 1898-1900.
- Bird MA, Amjadi D, Behrns KE. Primary splenic lymphoma complicated by hematemesis and gastric erosion. South Med J 2002;95(8): 941-942.
- Blanchi A., Bour B, Alami O. Spontaneous gastrosplenic fistula revealing high-grade centroblastic lymphoma: endoscopic findings. Gastrointest Endosc 1995;42(6): 587-589.
- Choi JE, Chung HJ, Lee HG. Spontaneous gastrosplenic fistula: a rare complication of splenic diffuse large cell lymphoma. Abdom Imaging 2002;27(6): 728-730.
- Dellaportas D, Vezakis A, Fragulidis G, Tasoulis M, Karamitopoulou E, Polydorou A. Gastrosplenic fistula secondary to lymphoma, manifesting as upper gastrointestinal bleeding. Endoscopy 2011;43 Suppl 2 UCTN: E395.
- Ding YL, Wang SY. Gastrosplenic fistula due to splenic large B-cell lymphoma. J Res Med Sci 2012;17(8): 805-807.
- Favre Rizzo J., López-Tomassetti Fernández E, Ceballos Esparragón J, Santana Cabrera L, Hernández Hernández JR. Massive upper gastrointestinal bleeding secondary to gastrosplenic fistula. Rev Esp Enferm Dig 2013;105(9): 570-871.
- Garcia Marin A, Bernardos García L, Vaquero Rodríguez A, Menchén Viso L, Turégano Fuentes F. Spontaneous gastrosplenic fistula secondary to primary gastric lymphoma. Rev Esp Enferm Dig 2009;101(1): 76-78.
- Harris NL, Aisenberg AC, Meyer JE, Ellman L, Elman A. Diffuse large cell (histiocytic) lymphoma of the spleen. Clinical and pathologic characteristics of ten cases. Cancer 1984;54(11): 2460-2467.
- Jain V, Pauli E, Sharzehi K, Moyer M. Spontaneous gastrosplenic fistula secondary to diffuse large B-cell lymphoma. Gastrointest Endosc 2011;73(3): 608-609.
- Kerem M., Sakrak O, Yilmaz TU, Gultekin FA, Dursun A, Bedirli A. Spontaneous gastrosplenic fistula in primary gastric lymphoma: Surgical management. Asian J Surg 2006;29(4): 287-290.
- Khan F, Vessal S, McKimm E, D'Souza R. Spontaneous gastrosplenic fistula secondary to primary splenic lymphoma. BMJ Case Rep 2010.
- Maillo C Bau J. Gastrosplenic and thoracosplenic fistula due to primary untreated splenic lymphoma. Rev Esp Enferm Dig 2009;101(3): 222-223.
- Moran M, et al. Spontaneous Gastrosplenic Fistula Resulting From Primary Gastric Lymphoma: Case Report and Review of the Literature. Balkan Med J 2011;(28): 205-208.
- Puppala S, et al. Spontaneous gastrosplenic fistula in primary gastric lymphoma: case report and review of literature. Clinical Radiology Extra 2005;60(2): 20-22.
- Rothermel LD, Chadwick CL, Thambi-Pillai T. Gastrosplenic fistula: etiologies, diagnostic studies, and surgical management. Int Surg 2010;95(3): 270-272.
- Cary ER, Tremaine WJ, Banks PM, Nagorney DM. Isolated Crohn's disease of the stomach. Mayo Clin Proc 1989;64(7): 776-779.
- Krause R, Larsen CR, Scholz FJ. Gastrosplenic fistula: complication of adenocarcinoma of stomach. Comput Med Imaging Graph 1990;14(4): 273-276.
- Martinez JD, Moya L, Hernández G, Viola L. Gastrosplenic fistula secondary to gastric adenocarcinoma]. Rev Gastroenterol Peru 2015;35(2): 165-167.
- Pizzirusso F, Gillet JP, Fobe D. Isolated spleen metastatic involvement from a colorectal adenocarcinoma complicated with a gastrosplenic fistula. A case report and literature review. Acta Chir Belg 2004;104(2): 214-216.