Figure 2. ETT is entering directly through the injury into the left main bronchus.
Discussion
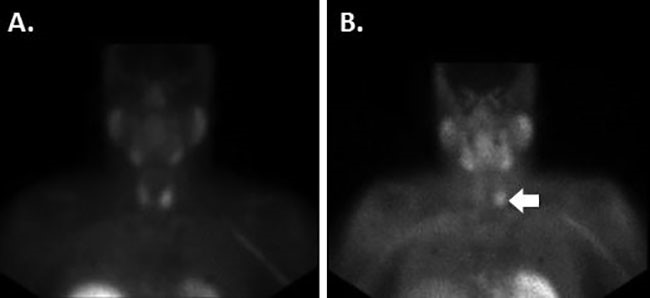
Blunt tracheobronchial injuries are uncommon and often lethal.1 The mortality rate for blunt injuries approaches 63 percent versus 13 percent for penetrating injuries. Moreover, blunt mechanisms of injury and the need for an emergent airway are independent predictors of mortality.2 Patients with distal tracheobronchial injuries classically present with subcutaneous emphysema and pneumothorax on chest radiograph. Our patient’s radiograph revealed subcutaneous emphysema and a deviated trachea (Figure 1). Additionally, our patient presented with a unique clinical sign rarely described in the literature as the “bullfrog effect.” This description is when the skin over the neck rises during inspiration and retracts during expiration.3 The deviated intrathoracic trachea, subcutaneous emphysema, and bullfrog effect heightened our index of suspicion for a tracheal injury, and thus led to emergent transport to the operating room. We theorize that as our patient’s intrathoracic rupture was contained in his mediastinum, his concomitant cervical transection accounted for the bull frog effect during his respirations.
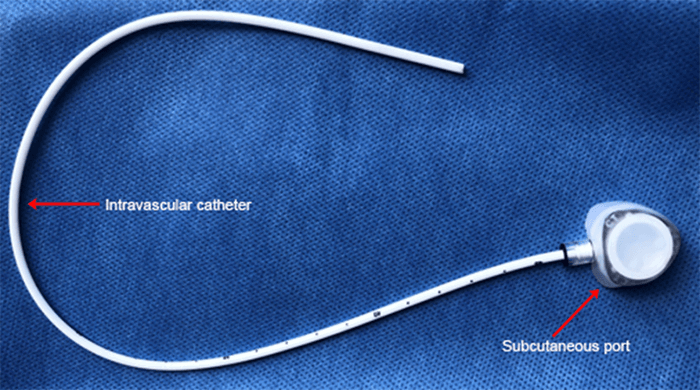
Once a tracheobronchial injury is suspected, securing the airway is a critical step in the management of the patient. Endotracheal intubation or creation of a surgical airway by directly intubating the tracheal injury are both acceptable techniques. Initially, an awake fiber optic intubation was attempted, but this step failed. A second orotracheal intubation was attempted; however, bronchoscopy through this ETT revealed abnormal anatomy, and we suspected the bronchoscope was in the mediastinum. In this particular case, performing a cricothyroidotomy would have placed us above the injury, delaying definitive airway. Our suspicion of intrathoracic airway injury coupled with worsening hypoxia and hypotension prompted us to perform a clamshell thoracotomy. In a retrospective study of blunt tracheobronchial injuries (n=259), right-sided bronchial injuries were more common (47 percent versus 32 percent) and were associated with a higher mortality rate (16 percent versus 8 percent, p=0.004) when compared to the left side. Furthermore, the mortality of patients with a ruptured trachea was 26 percent.4 For confirmed right sided injuries, a right posterolateral thoracotomy is the preferred approach. The distal left main stem bronchus is best approached through a left posterolateral thoracotomy.5 We elected to perform a clamshell thoracotomy in this scenario due to the possibility of additional associated injuries and our belief that traumatic arrest was imminent. A key step during this exposure is retracting the right lung medially and dividing the azygos vein. This allows for dissection of the tracheoesophageal groove and exposure of the distal trachea and right main bronchus.
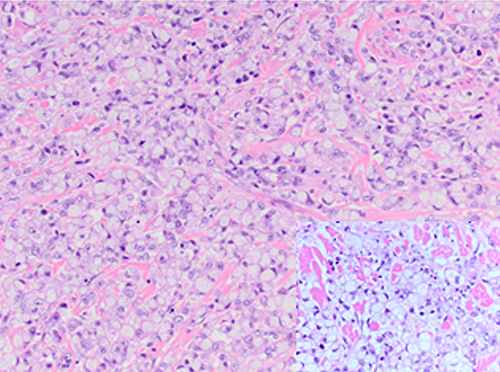
Once the airway is secure, defining the location and extent of the injury is the next critical step. More than 80 percent of blunt tracheobronchial injuries occur within 2.5 cm of the carina.6In our patient, we found a complex injury consisting of a long posterior tracheal laceration that extended cephalad up to the second ring in the neck where the trachea was additionally transected. We consulted with cardiothoracic surgery to assist, and our incision was extended cephalad via a median sternotomy. Some authors recommend a cervical incision for proximal tracheal injuries and a median sternotomy for suspected great vessel injuries.5,6 Once we located the proximal tracheal transection, repair of the injury was performed with an end to end anastomosis of the proximal trachea and by primary repair of the distal posterior trachea. We then passed a Cook catheter through the repair and advanced an ETT over it. The thoracotomy was closed, and the patient was transported to the surgical intensive care unit for further resuscitation.
Our patient then had a prolonged hospital course and developed acute respiratory distress syndrome (ARDS). He additionally developed a tracheoesophageal fistula and a mediastinal abscess that was subsequently treated with a stent and a right VATS to drain the abscess. He was discharged to an LTAC a month after his injury and then was discharged home. There is a paucity of data regarding the long-term morbidity and mortality for blunt tracheobronchial injuries. In a retrospective series of 32 patients, Baci et al reported a 30 percent mortality for patients with blunt tracheal injuries. The mean follow-up for this series was 11.8 months. Three patients developed tracheal stenosis. The majority of patient mortality was attributed to complications from ARDS.7
Conclusion
Tracheobronchial injuries are uncommon and often lethal. Astute clinical exam, rapid airway securement, and adequate surgical exposure are critical to identify and repair these injuries.
Lessons Learned
Identification of extensive subcutaneous emphysema of the upper chest and neck are critical clues for a major airway injury. An airway can be secured by passing an ETT directly through the injury in the neck or the chest. Division of the azygos vein is a key maneuver for exposure of the posterior mediastinum.
Authors
Carlos H. Palacio, MDa; Matthew J Wall, MD, FACSb; S. Rob Todd, MD, FACSb; and Stephanie D. Gordy, MD, FACSb
Correspondence Author
Dr. Carlos H. Palacio
Trauma and Acute Care Surgery
Michael E. DeBakey Department of Surgery
Baylor College of Medicine
One Baylor Plaza, Room 404D
Houston, Tx 77030
United States
713-798-6078
chplmd@gmail.com
Authors Affiliations
a Ben Taub Hospital, 1504 Taub Loop, Houston, Texas 77030 United States
b Michael E. DeBakey Department of Surgery, Baylor College of Medicine, One Baylor Plaza, MS 390, Houston, Texas 77030, United States
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Cassada DC, Munyikwa MP, Moniz MP, et al. Acute injuries of the trachea and major bronchi: importance of early diagnosis. Ann Thoracic Surg 2000; 69:1563-1567.
- Bhojani RA, Rosenbaum DH, Dikmen E, et al. Contemporary assessment of laryngotracheal trauma. J Thorac Cardiovasc Surg. 2005; 130(2):426-43.
- Sanchez LD, ban KM. A 29 year old man with subcutaneous emphysema of the neck following blunt trauma. Intern Emerg Med. 2007; 2:50-52.
- Kiser AC, O’Brien SM, et al. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg. 2001; 71:2059-65.
- DuBose JA, O’Connor JV, Scalea TM. Lung, Trachea, and Esophagus. In: Moore EE, Feliciano DV, Mattox KL, ed. Trauma, 8e. New York, NY: McGraw-Hill; 2017.
- Johnson SB. Tracheobronchial injury. Semin Thorac Cariodvasc Surg. 2008; 20(1):52-57.
- Balci AE, Eren N, Eren S, Ulku R. Surgical treatment of post-traumatic injury tracheobronchial injuries: a 14-year experience. Eur J Cardiovasc Surg. 2002; 22:984-989.