SAN DIEGO: To aid in decision-making processes and increase awareness around palliative care in the Surgical Intensive Care Unit (SICU), a research team at the University of North Carolina at Chapel Hill (UNC-Chapel Hill) has developed a screening tool to identify—within seconds—patients who may benefit from palliative care consultations or goals of care discussions. Their research findings, presented at the Scientific Forum during the American College of Surgeons Clinical Congress 2022, show that the screening tool successfully identified SICU patients who were later deemed candidates for palliative care by their medical team.
As a general and trauma surgeon, Trista Day Snyder Reid, MD, MPH, FACS, an assistant professor of surgery at UNC Health, and the study’s medical advisor, explained that she often witnesses medical teams and families make agonizing decisions for patients in the SICU. When aggressive medical interventions will not improve outcomes or extend life, palliative care treatment, which focuses on symptom management and supportive communication, may improve a patient’s quality of life. Unfortunately, a medical team may hesitate to collectively identify appropriate patients or may refer patients to palliative care late in their SICU stay, increasing the burden and stress on the patient and their families.
“One of the things that we found at our institution was sometimes we would involve palliative care, but it would happen way down the line when the patient had been in the SICU for a long time already,” Dr. Reid said. “We want palliative care discussions to be happening sooner. And even if we’re not involving palliative care, we want goals of care discussions to happen early so the family has a rapport with the medical team and understands that their family member is really sick.”
Across hospital systems, screening criteria and access to palliative care vary. Research has shown that offering palliative care consultations early in an ICU stay can improve quality of life and even reduce the lengths of stay in the ICU.1 However, integrating palliative care into hospital systems remains challenging due to a lack of resources and insufficient training, among other factors.2
Study details
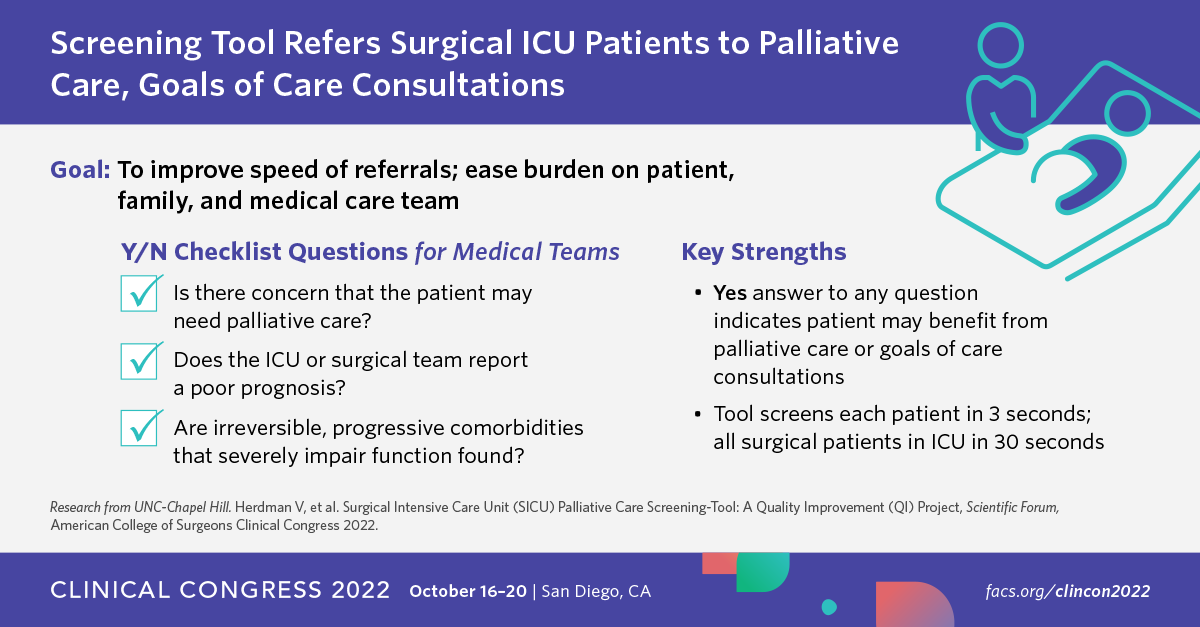
The UNC researchers initially developed a screening tool with 12 “yes/no” questions with input from SICU and palliative care physicians, nurses, and advanced practice providers. Fourth-year medical students at UNC-Chapel Hill completed the questionnaire after receiving feedback from the SICU medical team. Any question where the team answered “yes” was deemed a positive indicator that the patient would benefit from a palliative care consultation with a specialist or a goals of care discussion with the surgical team.
Three iterations of the screening tool were developed using the Plan-Do-Study-Act (PDSA) method before selecting three questions that the researchers found best correlated with a positive indicator:
- Any team member (nursing, physician, pharmacist, etc.) expresses concern the patient may need palliative care.
- ICU or surgical team answers ‘no’ to the question: “Would you be surprised if this patient died?”
- Comorbidities: irreversible, progressive, or untreatable, severely impairing function.
If yes was answered to any of the three checklist questions, the researchers believed the patient would likely benefit from a palliative care consultation or goals of care discussion.
Key findings
- Screening tools from 282 patients in the SICU were recorded.
- Of those 282 patients, the screening tool successfully identified 22 patients, all of whom eventually received referrals for palliative care.
- Each patient could be screened in about three seconds; all patients in the SICU could be screened in about 30 seconds.
- The tool did not increase the burden on the palliative care team at UNC Health.
“The hope is that by using this screening tool, decisions traditionally made very late in the patient’s SICU stay, could be made much earlier,” said lead author Victoria Herdman, MD. Dr. Herdman was a fourth-year UNC-Chapel Hill medical student at the time of the study and is now completing her residency in cardiothoracic surgery at the University of Kentucky College of Medicine. “Physicians, physician assistants, nurse practitioners and nurses know early on who needs palliative care but sometimes that’s hard to jump into early in the stay. This screening tool is a way to guide everyone into it easier.”
The research was performed at a single site, but the team hopes to evaluate the tool within other ICU populations at UNC Health using a Quality Improvement process, possibly using an electronic medical record system or implementing it during daily rounds discussions with only one question. The study team also plans future research to analyze patient demographics to determine which marginalized populations are often left out of palliative care discussions. Simply discussing palliative care more often and educating team members and families, they said, can make a difference.
“I think as surgeons we tend to have a lot of ownership of our patients because they’re trusting us with their bodies. But I think that may also bias us a little bit in terms of palliative care. We hear the words ‘palliative care’ and may say, ‘Oh, no, no, no! We don’t want that. That’s like giving up on our patient,’” Dr. Reid said. “But the truth is, I think a lot of surgeons don’t truly understand the definition of palliative care—that the goal is to align what the patient wants with your treatments. Our long-term hope is to make discussions of palliative care more commonplace and to change the culture so that people feel comfortable involving palliative care, or at a minimum having a goals of care discussion, so that patients and their families understand all the possible treatment options.”
The study was supported by the UNC Institute for Healthcare Quality Improvement. Study coauthors are Casey Olm-Shipman, MD, MS, Winnie Lau, MD, Kyle Lavin, MD, Marshall W. Fritz, BS, and Geoffrey Orme-Evans, JD, MPH.