“Telemedicine is currently built as a physician platform,” Dr. Matthews said. “We changed it to be inclusive of nurses; we engaged our nursing staff into the platform so that they continue to do the same roles that they do in person.”
Days before the patient’s telemedicine appointment, a nurse calls to notify the patient the visit is being changed from an in-office to telemedicine, and then walks the patient through the connection process. On the day of the visit, the nurse calls again 15 minutes before the visit to review the chart, “just like they would if the patient was there in the office,” Dr. Matthews said.
About three and a half weeks into their telemedicine experience, the Wake Forest Baptist Health urology physicians see about 15 patient visits via telemedicine a day compared to 30 in-office visits, Dr. Smith added. Despite a lower total number of visits, Dr. Matthews noted that a high rate of new telemedicine patient visits convert to surgery scheduling. “Anecdotally, the efficiency from a surgical subspecialty perspective of the translation of new patient appointments to scheduling of future surgeries is currently 20 to 25 percent,” she said. “So a surgeon who’s not engaging in telemedicine is losing out on an opportunity to identify patients who will need surgery in the next two to three months.”
There have been barriers to wider implementation of telemedicine. Reimbursement for telemedicine services had been one, but in March the Centers for Medicare and Medicaid Services issued a waiver that removed payment restrictions. Another barrier can be technology. Small percentages of people still don’t have smartphones or home computers, and internet service can be limited, especially in some rural areas. Dr. Smith said that the group had concerns about some elderly patients not having access to technology. “However, they’ve been able to engage younger family members to help them with the technology, and actually we’ve had very good success with that,” she said. For patients who don’t have video capability, the CMS waiver accommodates voice-only visits.
In addition to Dr. Matthews and Dr. Smith, study coauthors are Anthony J. Atala, MD, FACS; Ryan Terlecki, MD, FACS; and Erin Kelly, MSN, ANP-BC, all with the department of urology at Wake Forest Baptist Health.
The authors have no relevant financial disclosures to report.
“FACS” designates that a surgeon is a Fellow of the American College of Surgeons.
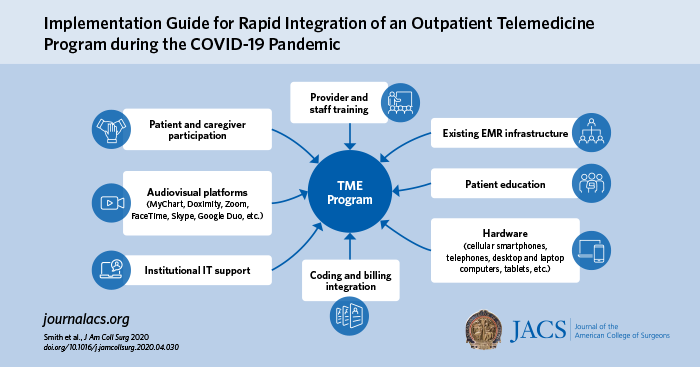
Citation: Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program amidst the COVID-19 Pandemic. Journal of American College of Surgeons. DOI: https://doi.org/10.1016/j.jamcollsurg.2020.04.030.