Children may be prescribed opioids to control severe pain resulting from their operations. Fatal poisonings from opioid overdoses are also increasing among both children and teens. Given the current rates of opioid abuse in the country, it is critical that patients understand how to safely use these medications and dispose of them once they are no longer needed.
Before your child’s operation, we encourage you to review the materials on this website. If you have questions, don’t hesitate to ask your child’s surgeon.
What are the goals of pain control?
The goals of pain control are to minimize pain, keep your child moving, help him or her resume normal activities, and help to heal.
What is safe and effective pain management?
Safe pain control is the use of medication and other therapies to manage pain with the least amount of side effects. Your surgical team will work with you and your child to:
- Screen for current opioid use and risk for overuse
- Use alternatives to opioids whenever possible
- Educate you about:
- Using the lowest dose of opioids for the shortest amount of time
- Safely storing and getting rid of any unused opioids
- Knowing and recognizing the signs of opioid overdose
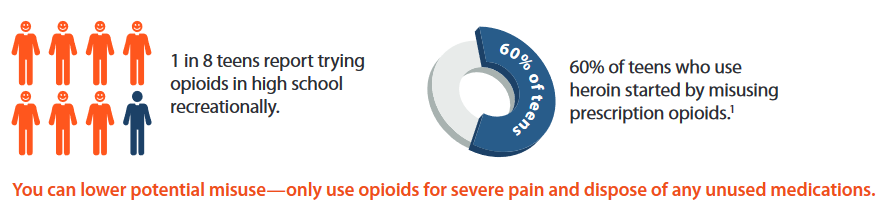
Why should I be concerned about opioid use in children and teens?
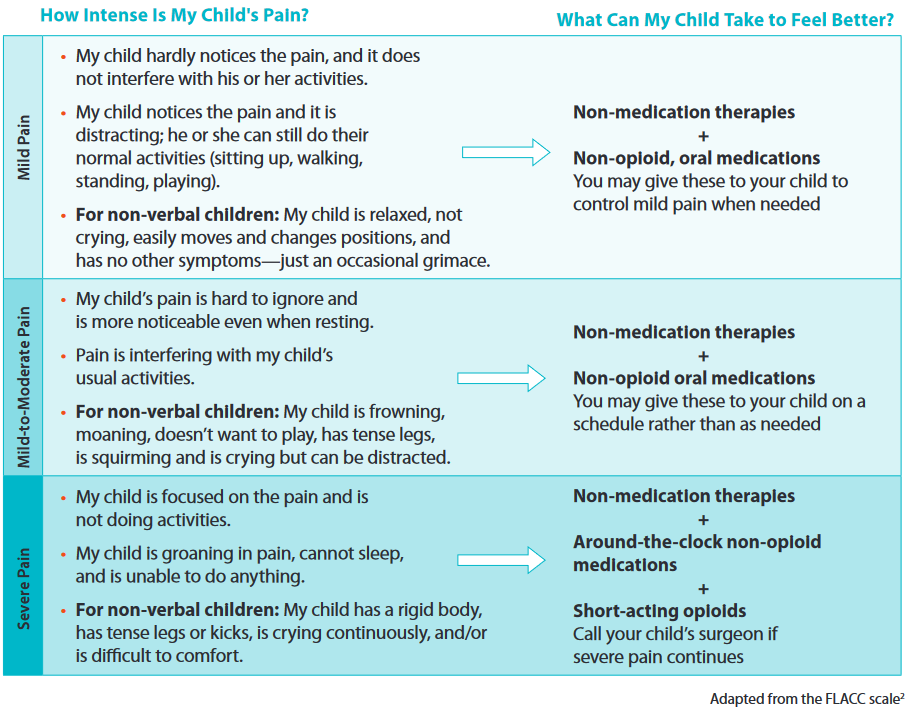
How can I help my child feel better?
Your child's pain may be controlled with a combination of non-medication therapies and non-opioid medications. For complex procedures, your child’s pain plan may also include opioids. After one to several days, the need for opioids will decrease. Use the guide below to help manage your child’s pain.
*Side effects reported in 3% or more of the patients in the study sample
Children with chronic pain or a history of prolonged opioid use will have an individualized plan for postoperative pain management.
How can opioids be used to safely manage my child's severe pain?
Your Child’s Surgeon May:
- Check if your child is at a higher risk for opioid misuse. Some questions the surgeon may ask:
- Does your child or a family member have a history of substance abuse or overdose?
- Is your child currently taking an opioid medication?
- Ask if your child has depression or attention deficit hyperactivity disorder (ADHD). Teens with depression and children/teens with ADHD have a higher risk of developing a substance use disorder (SUD) or misusing drugs, so screening is always recommended. Treating these disorders helps lower SUD risk.
- Review your child’s health history and other medications.
Your Child Should:
- Take the lowest dose possible.
- Never take more medication than prescribed.
- Never take opioids with antihistamines or sleep aids, sedatives or tranquilizers, anti-anxiety medications, muscle relaxers, cough medicines containing codeine, or another opioid. Combining these medications with opioids increases your child's risks of side effects.
- Never mix alcohol with NSAIDs or opioids.
- Never crush pills. This can speed the rate your child’s body absorbs the opioid and cause an overdose.
Parents: Communicate often with your child about his or her pain. Watch for adverse events or signs of misuse.
Can I wait to fill my child's opioid prescription?
Yes, you can wait to see if your child has severe pain before filling his or her opioid prescription.
Talk with your child’s doctor about this choice:
- Your child may not need the medications prescribed for opioid-related side effects (anti-nausea medication and laxatives).
- Be prepared with access to a 24-hour pharmacy in case your child's pain becomes severe in the middle of the night.
- Know that your child’s prescription is good up to 7 days after it is issued.
- Check if your child was given a long-acting anesthetic (stops pain at the wound or surgical site). This may help control your child’s pain for several days, and you may need fewer or no opioids.
How do I store and get rid of my child's leftover opioids?
For the safe storage of opioids:
- Store opioids in a secure location, preferably a locked cabinet or container.
- Keep medication out of reach of children and pets.
- Keep medication in its original container to avoid taking it by mistake.
- Keep track of the location and number of pills or liquid in the bottle.
Dispose of opioids as soon as they are no longer needed. You can locate a drug take-back program or safe drop site near you by visiting the U.S. Drug Enforcement Administration at apps2.deadiversion.usdoj.gov/pubdispsearch. If there is no disposal site near you, flush or pour any unused liquid down the drain. Mix unused pills with coffee grounds or kitty litter in a plastic bag, and then throw it in the trash.
What are the risks of my child becoming addicted to opioids?
Anyone who takes prescription opioids can become addicted. However, long-term use is rare when opioids are only taken to manage severe, postoperative pain. Opioids block pain and may give a feeling of euphoria (feel high). Taking prescription drugs to feel high is a type of prescription drug abuse.
Addiction involves seeking out the drug despite negative effects on your health, family, and work. Children may develop tolerance, meaning that over time you might need higher doses to relieve their pain. Children can develop physical dependence, meaning their body gets used to taking opioids and may have withdrawal symptoms when the medication is stopped suddenly. Tolerance and physical dependence put them at a higher risk for an overdose.
Withdrawal symptoms can include trouble sleeping, anxiety, irritability, racing heartbeat, and headaches. Withdrawal symptoms can be managed with medication and by gradually decreasing (tapering) your child’s opioid dose, but this should be guided by their doctor.
Check to see that your child’s pain is decreasing over the days following surgery. Call your doctor if you think your child is misusing their pain medication, experiencing tolerance, or experiencing physical dependence.
For questions and resources to help you or a loved one cope with a substance use disorder, visit the Substance Abuse and Mental Health Services Administration website at samhsa.gov or call the 24-hour helpline at 1-800-662-HELP (4357).