The Four Evils
The ACS BoR identified what it termed the “four evils” facing the profession, and these issues would remain a central focus of the ACS’s activities and a topic of intense discussion and debate for the better part of the century. The “four evils” exemplify the ethical challenges that emerged as a result of the changing social, economic, and institutional contexts of surgery in the early 20th century.
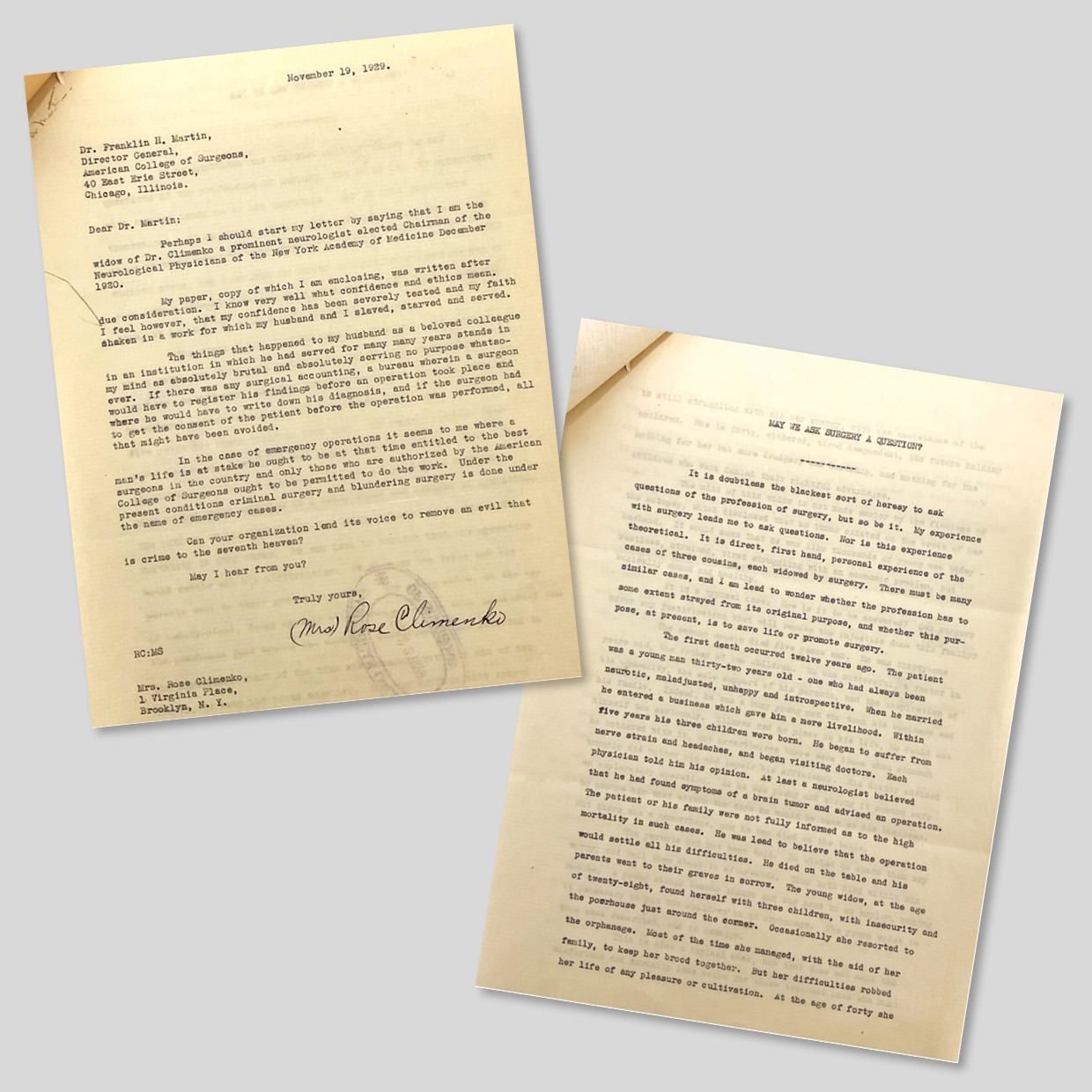
The ACS Archives provides a unique window into the development of surgical ethics, offering a more complete picture of the discussions surrounding complex ethical issues than can be surmised from public announcements and newspaper articles. Unlike public presentations, where the College leadership must present their consensus on any given issue, private correspondence allows members to discuss their differences of opinion more freely.
The College’s approach to each issue generally followed a similar pattern: defining the problem, discussing solutions, and implementing strategies. But the process also was marked by unique challenges and debates specific to each issue. By examining the committee’s deliberations and responses to these four core issues, we were better able to understand the factors that influenced surgical ethics not only during this period but also today.
Unjustified Surgery
According to the BoR, “an unjustified operation is one in which either the indications were inadequate, or the procedure was one which is contrary to generally accepted practice.”
This issue exemplifies the ways in which surgery at the time was not as we know it today. Debates about “unnecessary surgery” these days have to do with whether a double mastectomy is indicated for unilateral breast mass or whether appendicitis should be treated with an appendectomy or antibiotics. However, at the time, the cases were much more complicated.
The gravity of this issue is best exemplified by a letter written to the BoR in November 1929 by Rose Climenko, the widow of a prominent neurologist in New York. After losing multiple family members to unnecessary surgeries, Climenko wrote a letter to the board, pleading that it act on the still highly prevalent issue of unnecessary surgical procedures.
In her letter, Climenko provided details of these cases. The first case, from 1917, involves a 32-year-old man who was “neurotic, maladjusted, unhappy, and introspective.” He suffered from nerve strain and headaches until a neurologist believed he had found symptoms of a brain tumor and advised an operation. The patient and family were led to believe the operation was fairly routine and that it would resolve the patient’s difficulties. They were not informed of the high mortality risk associated with such an invasive procedure. Not surprisingly, the man died on the operating table, and an autopsy revealed no tumor. Climenko posed poignant questions: “It is a typical case—how is it to be answered? Can surgery offer any justification that will remove the injustice done this family?”
The second case, from 1924, describes a 31-year-old father of two. Although generally healthy, he experienced stomach issues. A doctor advised an exploratory operation, assuring him it was safe and that he would be back to work within 10 days. Trusting in the procedure’s safety, the man did not inform his parents. However, during the operation, he suffered a hemorrhage and died on the table. Climenko noted that this, too, was a typical case. These two cases were just the first of two personal examples Climenko used to illustrate the human cost of unjustified surgery and to urgently plead for reform.
The ACS addressed these ethical challenges through massive undertakings, such as the standardization project. In 1920, the organization published a minimum standard for hospitals, which included requirements for organized medical staff, accurate record-keeping, and adequate facilities. The ACS also established guidelines for surgical practices.
These efforts by the College laid the groundwork for future programs, such as the National Surgical Quality Improvement Program, which aims to measure and improve the quality of surgical care in the US. What are now considered quality issues in surgical practice were not always seen as matters of ethics or even standard practice within the profession. The ACS’s initiatives played a crucial role in establishing and enforcing these standards, ultimately leading to improved patient care and outcomes.