Cancer Reporting Disruptions
In 2023, Dr. Lum and colleagues were able to, for the first time, evaluate a full year’s worth of mature and complete data (2020) from the NCDB to understand how cancer reporting was disrupted. Data from the NCDB are used for a variety of research topics and quality improvement measures. In many ways, the NCDB is like a calm body of water: patterns emerge, but large waves of fluctuations generally do not occur in the historically stable dataset.
However, as Dr. Lum and coauthors analyzed the data, they noticed a startling trend: In 2020, there was a 14.4% overall decline in the number of reported cancer cases in the NCDB compared with 2019, representing more than 200,000 fewer cancer cases than expected that were not diagnosed and/or treated at CoC facilities.5
The research, published in JAMA Surgery, also revealed that certain racial, ethnic, and age groups were less likely to be diagnosed with cancer and/or receive cancer care, potentially exacerbating existing health disparities in cancer treatment.
The report serves as a “cautionary tale” that the depth of disruptions caused by the pandemic may still be underreported, and the interruptions caused by the pandemic will impact any report that includes 2020 data for years to come, potentially making it more challenging for researchers to observe certain trends.
“My main takeaway is to really look under the hood when using and analyzing NCDB data that from here on out will include data from 2020,” Dr. Lum said. “Because what you assume is happening may not actually be happening, and you have to really take a deep dive into the treatment variables and particular disease process to understand how the pandemic affected cancer care in your program.”
Missing Cancer Diagnoses
What happened to those 200,000 missing patients will be an area to study for years to come as more data reveal the complexities of pandemic-related disruptions to cancer care. The NCDB, a joint project of the CoC and the American Cancer Society, collects more than 1.5 million new cancer cases each year, representing more than 70% of all cancer cases in the US. The true incidence and scope of disruptions may be even larger beyond the 14% drop, and only by analyzing data after 2020 will a more complete story unfold.
“If there’s one thing we know it’s that cancer is not one disease. Cancer is so many diseases across the board, so we can’t globally comment that cancer is one thing,” said Heidi Nelson, MD, FACS, former Medical Director of the ACS Cancer Programs. “The pandemic is over; nobody wants to look back. But we have to understand what happened to 2020 data and other years of the pandemic as lessons learned and because it could have a downstream impact on all cancer programs.”
Dr. Nelson coauthored the JAMA Surgery study with Dr. Lum and has co-led other research looking at the long-term effects of the pandemic on cancer care. So far, many studies have explored the way the pandemic uprooted the healthcare system, including cancer care, but the true size and scope of the disruptions remain unknown, especially with studies involving smaller patient populations or those focused on regional variances or specific cancer types.
In October 2023, ACS scholars published research in JAMA Network Open looking at accessibility, availability, and utilization (defined by treatment modality and hospital type) of cancer treatment in 2020 compared with 2018 to 2019.6 The study looked at NCDB data from patients older than 18 who were newly diagnosed with cancer and treated at CoC-accredited programs. According to the authors, the study is one of the largest, most comprehensive evaluations of cancer treatment during the pandemic to date.
The team found that patients diagnosed with cancer in 2020 had about the same access and availability to treatment compared with previous years, which they attributed to the steadfast efforts of healthcare providers who recognized the true scope of the global health crisis and ensured their patients newly diagnosed with cancer were able to get treated quickly.
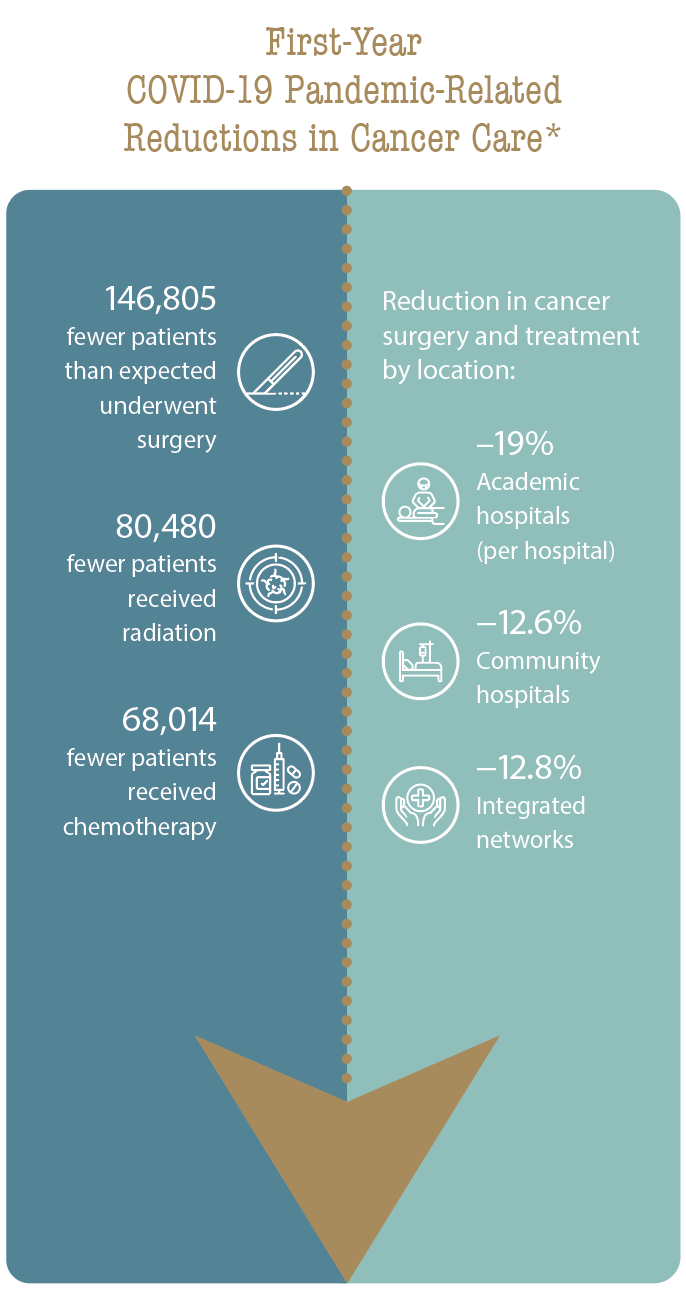
However, some notable disruptions still occurred, with the researchers finding that overall, fewer cancer patients than expected received chemotherapy and underwent surgery or radiation:
146,805 fewer patients than expected underwent surgery; 80,480 fewer received radiation; and 68,014 fewer received chemotherapy.
Academic hospitals experienced the greatest reduction in cancer surgery and treatment, with a decrease of approximately 19% per hospital compared with patients at community hospitals (−12.6%) and integrated networks (−12.8%).
The authors warned that these reductions could result in a large number of patients with untreated cancer, who could potentially face worse outcomes over the next several years. Separately, emerging research analyzing 2021 NCDB data suggests that cancer cases captured within the 2021 NCDB dataset did not return to pre-pandemic incidence levels, indicating that patients who went undiagnosed in 2020 were not captured the following year.7 This finding suggests that a considerable number of patients, especially vulnerable immunocompromised patients, may have died during the pandemic before their cancer was diagnosed.
Follow-up studies, experts said, are crucial to understanding the long-term effects of COVID-19 on cancer care and long-term survival outcomes. Related research on stressors of the pandemic also could be applicable in instances of other national emergencies, including severe weather events or natural disasters, that have the potential to disrupt or impact cancer care.
“The pandemic was a scary time because in the early months, we didn’t know how to manage patients with COVID,” said Lauren M. Janczewski, MD, MS, first author of the JAMA Network Open study and a Clinical Scholar in Residence within the ACS Cancer Programs.
Dr. Janczewski was a first-year general surgery resident at Northwestern University in Chicago, Illinois, at the start of the pandemic. Since then, much of her research at the ACS has focused on the impact of the COVID-19 pandemic on the delivery of cancer care.
“Patients’ families couldn’t see them. They were frustrated, scared, and upset, understandably. And from a healthcare provider standpoint, we were physically exhausted, and there was a fear of becoming ill. Thankfully we’ve been able to overcome a lot of those things,” she said. “But even though the public health emergency has been lifted, I think it’s important for us to take a deep dive and evaluate cancer data from the pandemic as more become available. By doing this research, the lessons learned from the pandemic are applicable on a much broader scale.”
Quantifying Missed Diagnoses and Screening Delays
Recognizing that in cancer treatment, the stage of diagnosis can have a dramatic impact on treatment options and survival outcomes for patients, the impact of missed diagnoses and screening delays related to the pandemic also remains an area of concern to surgeons and oncologists.
According to the 2023 Annual Report to the Nation on the Status of Cancer released by the National Cancer Institute (NCI) in October, new diagnoses of six major cancer types in the US—colorectal, female breast, lung, pancreas, prostate, and thyroid—plummeted in early 2020, coinciding with the early months of the pandemic.8
In particular, rates of early stage (in situ or localized) cancer diagnoses were lower for all studied cancers: colorectal (16.3% lower), prostate (14.8%), lung (14.7%), thyroid (11.8%), pancreas (9.9%), and female breast (9%).
By July 2020, diagnoses of all these cancer types except prostate cancer returned to pre-pandemic levels, but “these missed opportunities for early cancer detection are alarming, particularly for those vulnerable populations that continue to face significant barriers in accessing cancer care,” Monica M. Bertagnolli, MD, FACS, said in a statement9 when she was director of the NCI; she now is director of the National Institutes of Health.
For many, the report highlights an urgency to encourage patients to stay up to date on their screening tests and for surgeons to remain aware of a potential uptick in more advanced cancers as screening delays subside and a backlog of patients are treated.
Even with the public health emergency lifted, the impact of screening delays from the pandemic may cause a much greater impact on the medical community in future years, particularly on surgical oncologists, noted Teviah E. Sachs, MD, MPH, FACS, an associate professor of surgery at the Boston University Chobanian and Avedisian School of Medicine and chief of the Section of Surgical Oncology at Boston Medical Center in Massachusetts.
“While the medical system as a whole experienced an incredible burden from the COVID-19 pandemic, now we’re going to see a much different burden present itself due to delays in cancer screening,” he said.
Dr. Sachs coauthored research, published in the Journal of the American College of Surgeons in September 2023, that quantified the number of missed diagnoses of lung, breast, and colorectal cancers using NCDB data.10 The team’s predictive statistical model also included U.S. Census Bureau data to adjust for cancer cases not included in the NCDB.
The team analyzed data from 1,707,395 lung, 2,200,505 breast, and 1,066,138 colorectal cancer patients and found significant differences between the observed cancer rates in 2020 compared with predicted 2020 rates based on historical data from 2010–2019:
- Colorectal cancer: observed incidence decreased by 18.6%
- Lung cancer: observed incidence decreased by 18.1%
- Breast cancer: observed incidence decreased by 14.6%
“I think the magnitude of difference that we saw was surprising. Anecdotally, from working in hospitals and being first responders during the pandemic, you saw all of this but to be able to quantify it and see that it was actually at this magnitude was pretty remarkable,” said first author Kelsey S. Romatoski, MD, a surgical outcomes analysis and research fellow at Boston Medical Center and a general surgery resident at Beth Israel Deaconess Medical Center in Massachusetts.
Like Dr. Janczewski, Dr. Romatoski was in her first year of surgical residency in 2020. One of the things she said she remembers most is the fear many cancer patients expressed to her and fellow healthcare providers in moments of candor: Were they on the same floor as COVID patients? Has anyone around them been in contact with COVID patients?
“Cancer patients are already immunocompromised, so to add COVID on top of that, everybody was just so scared,” she said. “Looking at the patients, it was very difficult to realize that you didn’t know how to help them. A lot of patients died alone. It was very, very sad.”
For the next phase of her research, Dr. Romatoski aims to investigate how the pandemic impacted cancer diagnoses in the years after 2020 and if the drops seen in predicted versus observed diagnoses were sustained.
“If we’re anticipating that we may see higher stages of disease, how do we combat that and serve our patients the best?” she asked. “I still think it’s important to look back at COVID and put the data in context as more come out. The data are going to be very instrumental in predicting as much as we can into the future about what we’re going to see so that we can better prepare for it, train for it, and be ready to give patients optimal care.”
“Something like this could also happen again,” she added, “so I think it’s important to study those stresses within the healthcare system to adapt and make changes for future events.”
Cancer care team members are invited to come together and discuss the current state of cancer care at the ACS Cancer Conference in Austin, Texas, from February 22–24: www.facs.org/cancerconference.