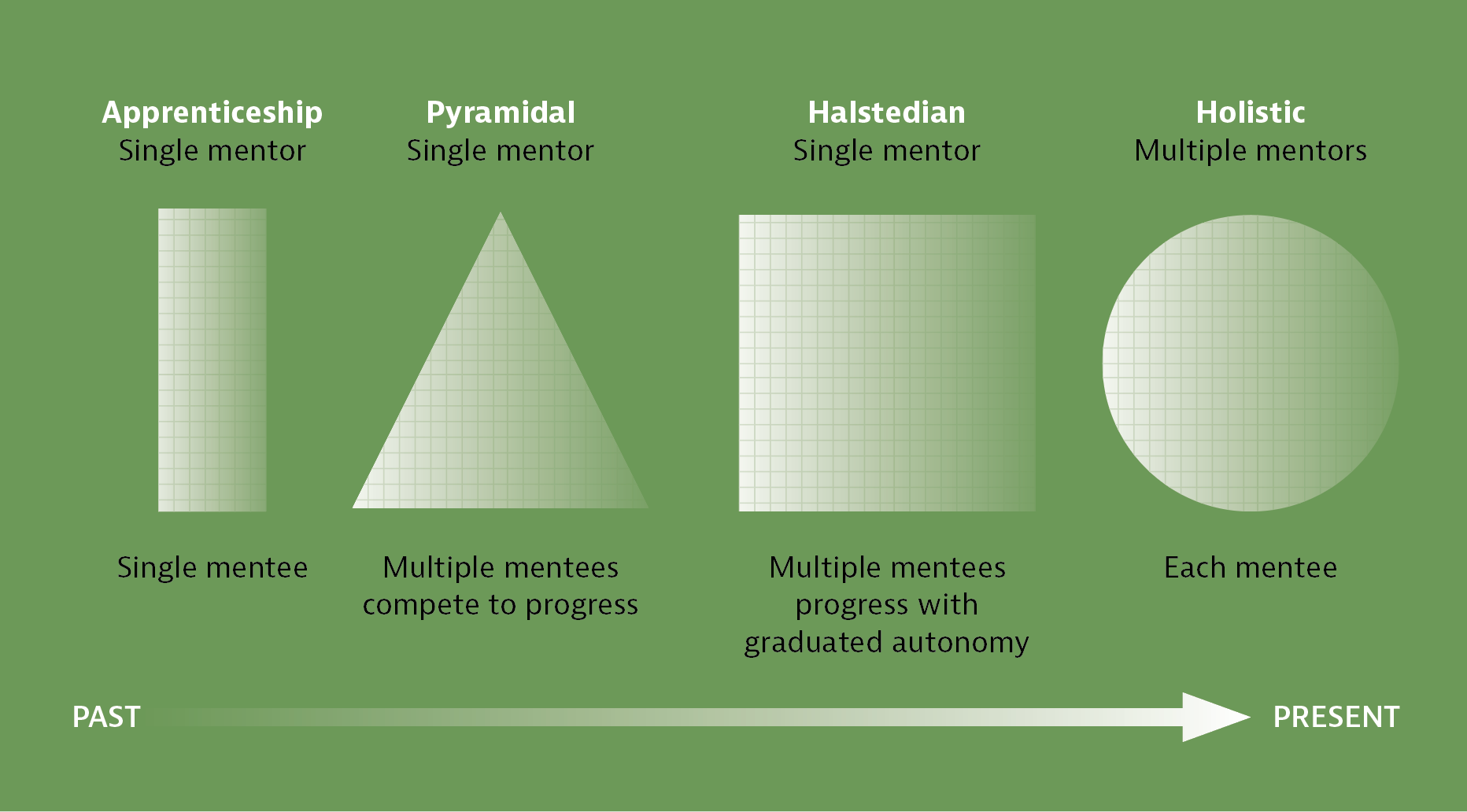
To look toward the future, we must understand our past—and the history of surgical education features milestones highlighting significant evolution.
In the mid-16th century, medical apprentice training began at around 13 years of age under a single mentor. This process involved direct observation and imitation of skills in a clinical environment for 5 to 7 years, which was followed by independent practice. There was no regulation on the requisite skills, structure of training, or oversight after independent practice.
Over time, the development of the Halstedian pyramidal, graduated autonomy residency model, and the formation of medical boards provided a necessary structure for surgical training. The evolution of standardization across hospitals and residency review committees and a shift to competency-based education have propelled us into the modern era.1
So, where do we go from here? The future of surgical education depends on surgeon leaders recognizing the challenges inherent in acquiring a massive amount of requisite knowledge and skills in an expedited amount of training time.
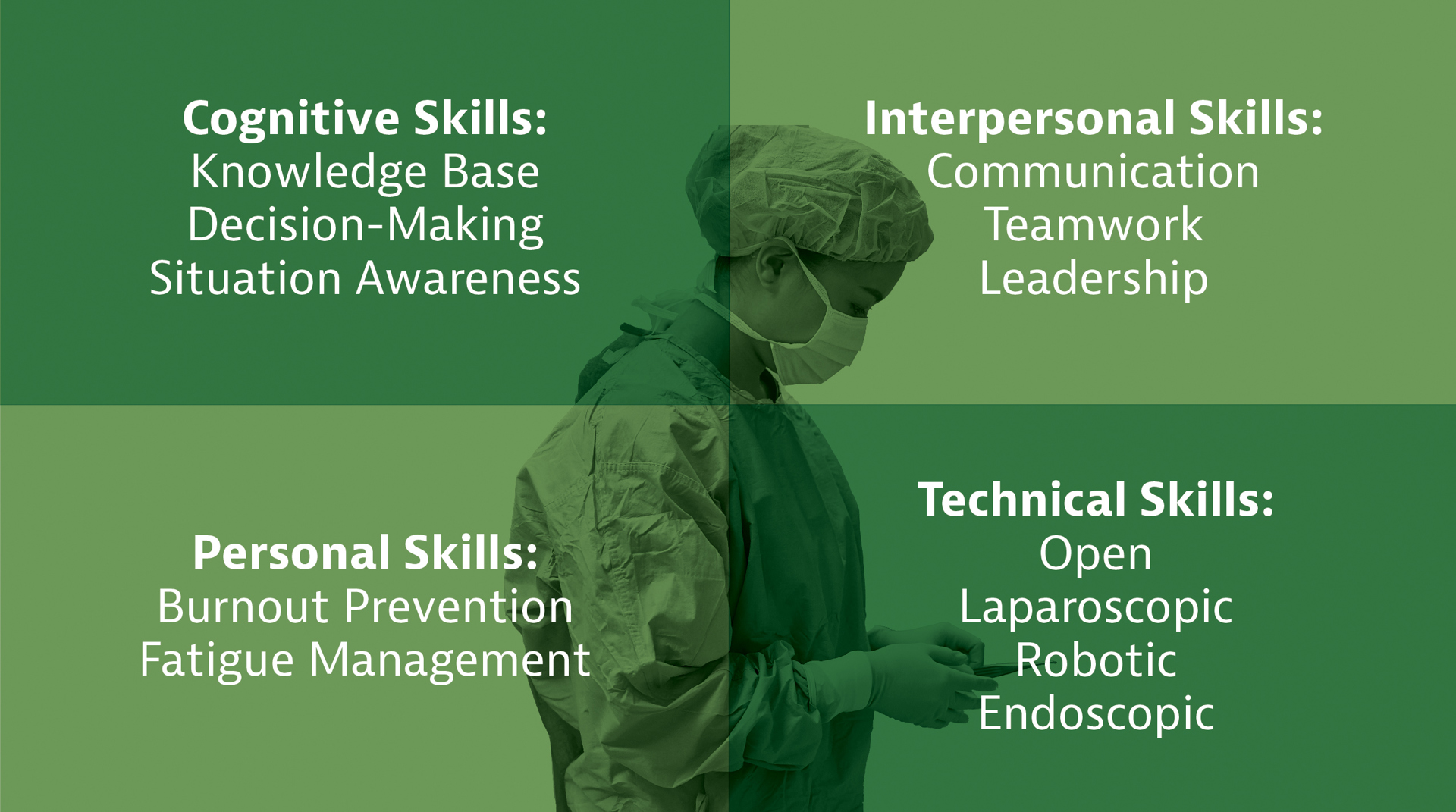
Rather than a linear “see one, do one, teach one” model, trainees are expected to evolve in multiple domains simultaneously to become well-rounded physician surgeons (see Figure 1). Surgical educators will need to plan beyond acquisition of technical skills and medical knowledge to emphasize the value of ongoing self-reflection and feedback, increase specialized certification, and encourage the development of nontechnical skills.
We will see another major shift in the training model, moving from assessing the adequacy of training based on time and case numbers, toward a full holistic review of how the trainee performs at all core competencies in the setting of the larger healthcare system.
Developing Technical Skills
As the modern world has evolved with the growing integration of technology in daily life, so has medicine, surgery, and surgical education. Previous skill acquisition was relegated to the “present” with apprenticeship models or even simulation practice.
The future integration of technology will allow us to “train from our past” by making resources to record, analyze, and review procedures universally. Indeed, the current applications of multimedia-based training have been found to significantly improve the surgical performance of fellows and the education of students.2
These systems will grow to be seamlessly integrated into training and provide a variety of benefits. Video and audio recordings can be obtained for entire cases, and editing software may be used to condense these videos into highlights that focus on key aspects of a procedure.
Trainees typically will have immediate access to data that will facilitate self-reflection with longitudinal records to monitor their progression. Furthermore, these videos will allow for feedback and coaching mechanisms from surgical educators regardless of time or space and will allow the trainee to develop higher-level competencies targeted toward certification and, ultimately, quality improvement.
Technology in the operating room (OR) also has been applied to surgical safety with the creation of the OR Black Box. The term “black box” comes from the aviation industry where technology is used to collect comprehensive flight data and real-time monitoring. From this information, risk can be mitigated, and accidents can be reviewed to develop strategies to identify and avoid future events.
Our current model of operating room safety relies on subjective factors such as retrospective review and self-reported morbidities and mortalities. Going forward, identifying one’s objective metrics can be standardized with data collection from wall-mounted cameras, microphones, and video feeds from laparoscopic instruments for general surgery cases. Early studies found an average of 20 errors per case, usually during the dissection and reconstruction portion of cases, and an average of 138 auditory distractions.3
Future surgical trainees will be expected to master their technical skills using clinical and simulation training, supplemented by video-based review, in order to evaluate their performance while identifying areas for improvement. Current barriers for developing this process on a wider scale include the cost to integrate such technology and the acceptance of a coaching model of ongoing surgical training.
Assessing Technical Skills
As the number of technical competencies increases, so must the procedures for learning and for verification of these skills. While the Fundamentals of Laparoscopic Surgery (FLS) and Fundamentals of Endoscopic Surgery (FES) programs are now required for the General Surgery Qualifying Exam, there is no standardization for when these certifications should be completed or a consensus regarding the required surgical simulation curriculum.4
Moreover, comfort in a simulation environment can predict improved performance but not guarantee mastery of the operative environment for laparoscopic, endoscopic, or robotic procedures.
Indeed, there are subtle technical nuances that only are gained through supervised real-time operative exposure with appropriately increasing resident autonomy. To facilitate this learning curve, programs may lean toward an early introduction of the FLS and FES curricula, allowing more time for mastery of advanced skills through the remaining residency years and by increased faculty comfort levels regarding resident autonomy.
Simulation in surgical education needs to parallel the growth in the variety and sophistication of surgical technology over time.
Laparoscopic surgery has dominated procedures in private and academic centers; yet since its introduction in 2004, the FLS curriculum has not been adapted to parallel this increasing complexity. Recent evidence of a high FLS first-pass rate of 96% belies the need for curricula to match the increasing complexity of trainees’ laparoscopic case exposure and the skillset required of a graduating general surgery resident.5
Development or alteration of new modules, however, should carefully consider their value in lieu of a trainee’s clinical responsibilities, financial burdens, and mental well-being. Added certifications without appropriate educational value will, without a doubt, have a negative impact.
Importance of Soft Skills
The present shift to patient-centered healthcare will lead to the future reorientation of surgical education and the establishment of an ideal “professional” surgeon. There is growing awareness that these effective surgeons must possess nontechnical skills (NTSs) or soft skills to engage with patients and colleagues, and undergo formal training and assessment of NTSs.
NTSs have been defined in various ways, most commonly as “the cognitive and social skills that characterize high-performing individuals and teams.”6 These skills are frequently organized into three distinct categories: cognitive (e.g., decision-making, situational awareness); interpersonal/social (e.g., communication, teamwork, leadership); and personal (e.g., overcoming burnout, managing fatigue).
In the last decade, the importance of NTSs for patient care has been demonstrated extensively, with studies showing that the majority of surgical complications result from deficiencies in NTSs (e.g., communication breakdown) rather than technical errors.7
Formalized training and validated assessment tools of NTSs for surgeons and surgical trainees also have been studied. The most widely studied and validated tool is the Non-Technical Skills for Surgeons (NOTSS) system. A modified version of this framework, the NOTSS-US, has been studied as an assessment for trainees in the US.8
The NOTSS and NOTSS-US systems focus on four areas: situation awareness, decision-making, communication and teamwork, and leadership. Each of these categories is further broken down into specific elements (e.g., exchanging information, coping with pressure).
A trained rater uses this tool to assign the trainee a rating for each relevant skill per case after which feedback and discussion should identify areas for improvement. While NOTSS focuses on a surgeon in the operating room, other modified assessment tools have been developed to evaluate the surgical team as a whole (surgeon, anesthesiologist, and nurses) or a surgeon in the trauma resuscitation environment.
In trainee studies, the NOTSS-US was found to correlate with postgraduate year.9 This suggests that, similar to technical skills, there should be an expected graduated improvement of NTSs and formal incorporation into training. In the current framework, NTSs fall within the individual competencies of professionalism and interpersonal communication milestones that residents are expected to aim for prior to graduation. As the transition to more holistic competency-based training occurs, NTSs will be incorporated into formalized training as a foundational part of surgical training within the next decade.
Paradigm Shift in Assessment
Our trainees are now expected to master open, laparoscopic, endoscopic, and robotic surgery. Additionally, they are expected to acquire an ever-expanding knowledge base and demonstrate leadership and communication skills. It is no longer feasible to rely solely on time in training or number of cases to assess a trainee’s readiness for independent practice.
So, how will we assess this “future surgeon” who is charged with mastering knowledge, technical skill, and soft skills? This assessment likely will come as the profession transitions into the new paradigm of Entrustable Professional Activities (EPAs).
EPAs initially were developed in the Netherlands for physicians to better determine their deficiencies in competencies. The EPA framework will launch as an adjunct to the established milestones from the Accreditation Council for Graduate Medical Education.
In 2020, five general surgery EPAs were piloted: evaluation and management of a patient with inguinal hernia; evaluation and managing of a patient with right lower quadrant pain; evaluation and managing a patient with gallbladder disease; evaluation and initial management of a patient presenting with blunt or penetrating trauma; and providing general surgical consultation to other healthcare providers.
Beginning in July 2023, these five EPAs and an additional 13 will be initiated in general surgery programs (see Table). Together, these 18 EPAs aim to assess the core competencies (knowledge, technical skill, and soft skills) in a standard holistic way.