The coronavirus 2019 (COVID-19) pandemic is a public health crisis with a societal impact that reaches beyond the damage of the highly contagious illness itself. Quarantine, shelter-in-place orders, social distancing, and travel restrictions all have proven to be indispensable measures in mitigating virus spread. However, these efforts have, in turn, created considerable challenges for the world population. The burden of COVID-19 extends far beyond infection and disease. Many individuals worldwide have endured social, financial, and psychological ramifications—leaving those affected by intimate partner violence (IPV) particularly vulnerable. Mandates enforced to save lives may ultimately endanger the lives of those at risk for IPV.
IPV is defined as physical violence, sexual violence, stalking, or psychological aggression by a current or former intimate partner.1 Despite increasing social media coverage and public awareness surrounding IPV, its prevalence continues to rise, with more than 10 million people in the U.S. enduring IPV annually.1 Every surgeon will encounter patients, peers, friends, and loved ones who have experienced IPV, regardless of whether IPV is identified as the mechanism of injury or goes unrecognized. IPV prevention involves maintaining a high index of suspicion for current and ongoing violence. Surgeons have an opportunity to save lives outside of the operating room when this level of awareness is maintained.
Patient demographics
IPV does not discriminate. It affects individuals of all ages, genders, races, ethnicities, socioeconomic classes, and education levels. Authors of the most recent National Intimate Partner Violence and Sexual Violence Survey (NISVS) reported that in the U.S., more than one-third of women and up to one-third of men experience IPV at some point in their lifetime.1 Although both men and women are affected by IPV victimization, women more frequently experience severe consequences of IPV and suffer life-threatening injuries.1 The disproportionate impact of IPV on women is apparent in homicide data, which indicate that 42 percent of female murder victims are killed by an intimate partner, while 5 percent of men sustain fatal injuries with an intimate partner as the perpetrator.2,3 Nearly 50 percent of women murdered by an intimate partner have a documented emergency department (ED) visit within two years prior to their death.3 These patients often present with traumatic injuries, which provide surgeons with an opportunity to break the cycle of violence.
Injury patterns
IPV injury pattern recognition has the potential to significantly improve detection rates and promote appropriate management and support. Maxillofacial injuries account for 81 percent of IPV-related injuries, and 67 percent of facial fractures sustained secondary to IPV involve the middle third of the face.4 Orbital and ocular injuries account for 45 percent of IPV-related injuries.5 Nasal fractures (40 percent) are the most common assault-related facial fracture in women, while the bony orbit and the zygoma are fractured in 18.9 percent and 16.5 percent of cases, respectively.4
Pattern recognition can also be applied to laterality and mechanism of injury in order to discern between assault-related injuries and other sources of facial trauma. Eighty-one percent of facial fractures and 85.7 percent of zygoma fractures that originate from IPV are left-sided. Blunt trauma with a closed fist is the mechanism of injury in most IPV cases. In analyzing these patterns, it is important to consider that 90 percent of the population is right-handed; as a result, a successful blow most often will be delivered to the left side of the face.4,6,7 These details may seem insignificant on their own, but when combined, the patterns can paint a more accurate picture of the circumstances leading to injury. These observations are particularly useful in cases where the history provided by the patient is inconsistent with the injuries sustained. Individuals who experience IPV may be hesitant to share the true cause of injury due to fear of retaliation from their partner or a false belief that the abuse is their own fault.
Detection and management
IPV is underreported and often goes unrecognized by family members, friends, and health care providers, possibly because of a low propensity of patients who experience IPV to disclose abuse when not prompted to share this information. Research shows that only one in four women patients will offer spontaneous testimony of an IPV incident.8
Patient surveys indicate that most female patients expect their health care provider to initiate the conversation surrounding IPV.8 Only 8 percent report feeling uncomfortable discussing IPV with their health care professional.8 Unfortunately, many health care professionals underestimate the prevalence of IPV and report low confidence in their ability to screen for IPV and make appropriate referrals to community-based agencies.6
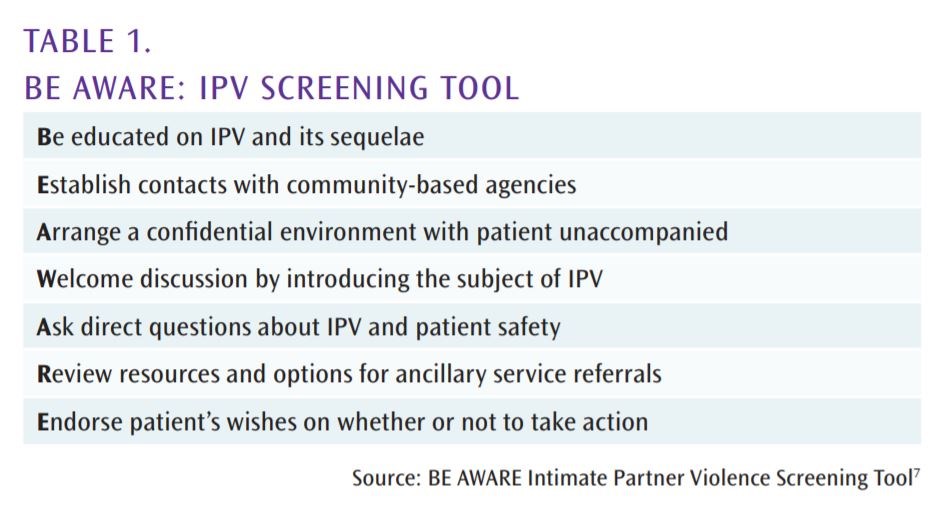
Surgeons must take action to disrupt the cycle of violence. Making detection and management of IPV a priority can save the lives of countless patients, peers, and loved ones. Educational instruction on direct questioning and community resources (see Table 1) will strengthen provider confidence in introducing IPV into the conversation during a patient encounter. Normalizing IPV discussion and promoting safe disclosure should become standard practice in health care.
Screening paired with appropriate referral and access to community resources has proven to be a successful means of intervention by health care providers. Women who discuss IPV with their health care provider are 4 times more likely to use an intervention and 2.6 times more likely to leave an abusive relationship.9 A study conducted at an urban, academic Level I trauma center demonstrated that 84 percent of women patients who sustained injuries secondary to IPV examined in the ED agreed to speak with an in-house patient advocate. More than half of the patients who spoke to a patient advocate connected with a case manager and 49 percent of the patients who followed up with a case worker reported that they were no longer at risk for violence from their partner one year after the initial incident.10
Screening and referral
An IPV protocol (see Table 2) is optimized by creating a health care environment that promotes safe disclosure, pairs screening and referral, and involves community-based services in responding to patients’ immediate and ongoing needs.7,11 Before screening for IPV, injuries should be addressed and appropriately managed. Before initiating the conversation, a confidential environment should be created with the patient unaccompanied. If the patient cannot be screened alone because a companion is reluctant to leave the patient’s side, the provider should notify the companion that the patient will need to be relocated temporarily for additional testing and provide reassurance that the patient will be directed back to the exam room after testing has concluded.11,12
Once the patient is relocated, introduce and normalize the subject of IPV with a statement such as, “I have some questions that I ask all of my patients because intimate partner violence is a common cause of serious injuries.” Then begin screening with a behavior-specific question, such as “Have you been physically, sexually, or emotionally harmed by an intimate partner?” followed by “Are your current injuries a result of abuse by an intimate partner?” 7,11,13 When a patient discloses IPV as the mechanism of injury, it is critical that the provider offers support and avoids statements that could alienate the patient, such as recommending that the patient leave their partner.7 Instead, respond compassionately by thanking the patient for sharing this information, reassuring the patient that the violence is not her or his fault, and asking the patient if she or he feels safe going home.7,11
The patient subsequently should be counseled with information that focuses on safety and health risks of IPV. This portion of the discussion is also an opportunity to ask about immediate safety concerns and develop “in case of emergency” plans. Providers should offer information on social work and counseling services, local shelters and agencies, as well as law enforcement, and provide a referral with the patient’s permission.7 At minimum, patients should be briefed on the prevalence of IPV and its related health risks. Patients should be provided with information on social services, the national domestic violence hotline 1(800)799-SAFE, and local crisis centers.
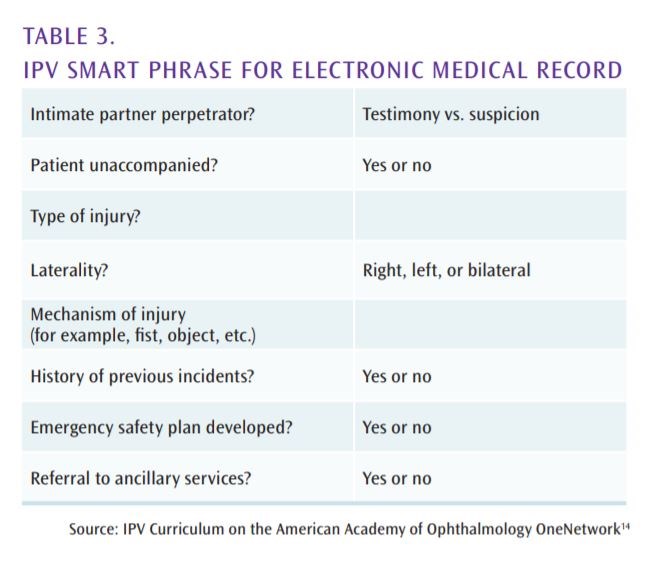
The entire patient encounter should be documented thoroughly and securely. Successful completion and proper documentation of IPV screening and management can be confirmed with an IPV smart phrase (see Table 3).
made available in the electronic medical record.14 Use of a smart phrase guides providers to indicate whether the patient gave verbal testimony regarding IPV as the source of injury or if screening was performed based on provider suspicion. The smart phrase reminds providers to conduct screening with the patient unaccompanied and to document important information such as type and laterality of the injury, mechanism of injury, and a history of previous incidents. It also serves as a reminder to develop a safety plan with the patient before the patient encounter is over and to make appropriate referrals to ancillary services. This information should be included in a protected event note so it is not visible through the patient portal, to discourage violent retaliation if discovered by the perpetrator.14 Close follow-up should be arranged after completion of screening and counseling.
Conclusion
The COVID-19 pandemic has heightened and renewed the public’s sense of concern for safety, especially for those affected by the virus. It has affected the physical, mental, and emotional health of the population at large and has exposed many health care inequities. COVID-19 has without a doubt changed the world, and with that, medical practice must evolve to accommodate evolving patient needs. The role of the surgeon in saving lives should not be limited to the boundaries of the operating room.
Surgeons must recognize the impact we have on every facet of care, especially during these uncertain times. IPV is a serious and underdiagnosed cause of traumatic injury and ED visits. Surgeons must be vigilant in identifying individuals at increased risk for injury secondary to IPV during the COVID-19 pandemic and thereafter. In doing so, we can make a difference in lives that will last long after discharge from the hospital. Understanding demographics and recognizing injury patterns consistent with IPV-related assault, in conjunction with the application of an IPV protocol, will help surgeons maintain the high index of suspicion necessary to promote the resolution of violence against patients, peers, friends, and loved ones.
References
- National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention. The National Intimate Partner and Sexual Violence Survey (NISVS) 2015 Data Brief. Available at: www.cdc.gov/violenceprevention/datasources/nisvs/summaryreports.html. Accessed August 4, 2020.
- Bridges FS, Tatum KM, and Kunselman JC. Domestic violence statutes and rates of intimate partner and family homicide: A research note. Criminal Justice Policy Review. 2008;19(1):117-130.
- Dearwater SR, Coben JH, Campbell JC, et al. Prevalence of intimate partner abuse in women treated at community hospital emergency departments. JAMA. 1998;280(5):433-438.
- Le BT, Dierks EJ, Veeck BA, et al. Maxillofacial injuries associated with domestic violence. J Oral Maxillofac Surg. 2001;59(11):1277-1283.
- Berrios DC, Grady D. Domestic violence. Risk factors and outcomes. West J Med. 1991;155(2):133-135.
- Saddki N, Suhaimi A, Daud R. Maxillofacial injuries associated with intimate partner violence in women. BMC Public Health. 2010;10(1):268.
- Cohen AR, Renner LM, Shriver EM. Intimate partner violence in ophthalmology: A global call to action. Curr Opin Ophthalmol. 2017;28(5):534-538.
- Hayden SR, Barton ED, Hayden M. Domestic violence in the emergency department: How do women prefer to disclose and discuss the issues? J Emerg Med. 1997;15(4):447-451.
- McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women’s receipt of interventions and improved health. Public Health Rep. 2006;121(4):435-444.
- Krasnoff M, Moscati R. Domestic violence screening and referral can be effective. Ann Emerg Med. 2002;40(5):485-492.
- Clark TJ, Renner LM, Sobel RK, et al. Intimate partner violence: An underappreciated etiology of orbital floor fractures. Ophthal Plast Reconstr Surg. 2014;30(6):508-511.
- Clark TJ, Renner LM, Sobel RK, et al. Ophthalmologist’s pocket guide to IPV. Ophthal Plast Reconstr Surg. 2014. Available at: https://cdn-links.lww.com/permalink/iop/a/iop_2014_03_05_shriver_oprs-d-13-00594_sdc1.pdf. Accessed August 4, 2020.
- Cohen AR, Clark TJ, Renner LM, Carter PC, Shriver EM. Intimate partner violence as a mechanism of traumatic ocular injury in women. Can J Ophthal. 2019;54(3):355-258.
- Cohen AR, Shriver, EM. Intimate Partner Violence (IPV). American Academy of Ophthalmology OneNetwork 2020. Available at: www.aao.org/resident-lectures-video/intimate-partner-violence-ipv. Accessed August 4, 2020.