Many residents interrupt their clinical training to pursue other professional interests full time. This article is intended for surgical educators involved in graduate medical education who are interested in supporting these residents as they transition back to clinical patient care. The objectives of this article are to describe:
- Describe the frequency and purposes of interrupted clinical training in general surgery residency
- Explore the potential challenges of residents returning to clinical training
- Share interventions and program practices that may support residents who are returning to clinical residency
A sizable fraction of general surgery residents interrupt their clinical training to pursue nonclinical endeavors, typically research activities. A 2009 survey of general surgery program directors revealed that 36 percent of surgical trainees interrupted their clinical training by one to three years to pursue full-time research.1 At that time, the majority of research residents were engaged in basic science research (72 percent) and the cost of these research fellowships was reportedly more than $40 million. New England residency programs have reported an even higher rate of clinical interruption, with more than 60 percent of residents participating in full-time research at some point during their residency training.2 In the past decade, some academic residency programs have mandated 100 percent of their trainees take dedicated time for research or other professional development activities such as obtaining advanced degrees or completing quality and safety fellowships. For residents who continue to pursue research full time, the breadth of research has expanded, with residents often focusing on developing research skills in health services or education research rather than basic and translational science. The overall purpose of these years has historically been to prepare trainees for careers as surgeon-scientists against a background of concern regarding the diminished participation of surgeons in federally funded research.3,4 With the pivot from viewing this time as "professional development" rather than purely "research," trainees frequently use these years of clinical interruption with an eye to careers in global surgery, administration, business, technology, and education, among others. In this article, we use the term "research resident" or "lab resident" to refer to all trainees who take time away from clinical residency to pursue these other professional interests.
Regardless of whether a trainee interrupts their clinical training to pursue research or other endeavors, there may be a cost to this time away from full-time patient care. Research residents report a subjective decline in their clinical skills, with residents who take more time for research more likely to report a decline in skill.5 Complex technical skills that had not been mastered prior to the research/professional development period may be particularly vulnerable to decay. At least one group has demonstrated that residents who interrupt their clinical training perceive a greater decline in technical skill and procedural knowledge for more advanced tasks, such as hand-sewn bowel anastomosis and laparoscopic ventral hernia repair, when compared to simpler tasks such as urinary catheterization.6 Faculty also perceive skills decay in residents who interrupt their clinical training. Attending surgeons report that, relative to their peers who progress through clinical residency uninterrupted, residents returning from a gap in clinical training demonstrate less technical skill, less confidence, and require more instruction, particularly for complex procedures.7
This perceived decline in technical skill and procedural knowledge may be a key motivation for residents to pursue moonlighting opportunities as they try to combat this decline in patient care skills. In a survey study of residents at a university-based residency program, 93 percent of residents reported one motivation to moonlight was to preserve clinical acumen.8 Furthermore, residents indicated strong agreement that any operative experience gained during moonlighting was valuable. While we did not identify any literature that demonstrates more objective measures of technical skills decay specifically for surgery research residents, there is evidence more broadly about trainees' technical skill decay across time.9
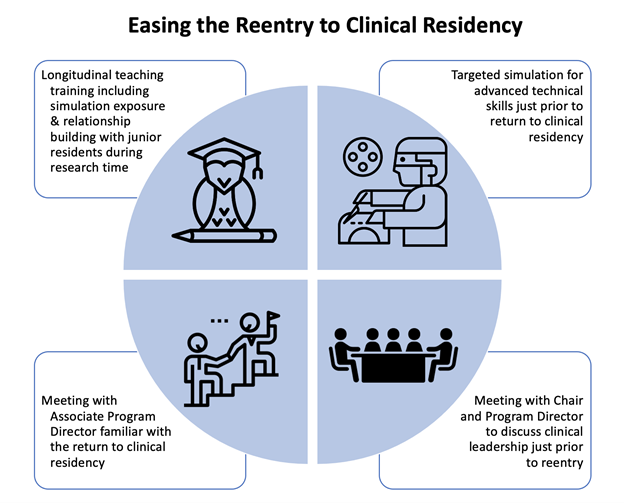
There has been limited work on formally supporting residents during clinical training interruptions or as they return to clinical residency, and no national program or curriculum exists to optimize the re-entry of residents to full-time patient care. At our institution, we have developed several structured interventions to support the reentry of residents who have chosen to take time away from clinical residency (Figure 1). Beyond the interventions described below, research residents are encouraged to remain active participants in the residency community by attending educational conferences and social events. and they are given a prominent role in intern recruitment due to their more flexible schedules. Research residents are also required to meet with the program director or an associate program director for a formal evaluation every six months to evaluate their progress toward their professional goals.
With regard to technical skills, the research residents at Massachusetts General Hospital (MGH) are supported both during their professional development years and just prior to the return to clinical residency. Research residents are offered the opportunity to participate in a longitudinal Research Residents as Teachers Program, in which they complete a half-day workshop led by a surgical educator on high-yield topics such as adult learning theories, giving feedback, and teaching technical skills.10 The residents then have an opportunity to teach in a variety of structured settings including medical student orientations and our weekly simulation curriculum for junior residents. While the original intent of the program was to develop the lab residents as teachers, participants describe that the program has a prominent "ripple effect" to other aspects of their development such as technical skill maintenance.10 By teaching in the longitudinal simulation curriculum, research residents have an opportunity to benefit from the faculty instruction provided at these sessions and practice advanced skills such as vascular anastomosis, hand-sewn bowel anastomosis, and advanced laparoscopic simulation. Participants also describe a greater sense of social connection to the clinical residents, which may facilitate their return to full-time clinical residency, especially in the role of team leader, because they have interacted with junior residents in the context of the simulation curriculum who they may not have otherwise met in the course of their research or other activities. While we have not formally studied faculty perception of residents who participate in this program relative to the residents who did not, we have anecdotally received feedback from attending surgeons that residents who frequently taught in the simulation lab exceeded their peers in technical skill upon return to clinical residency.
Our institution also offers lab residents targeted simulation sessions that are focused on practicing the higher complexity technical skills most relevant to their upcoming clinical rotations. At least two sessions are scheduled in the month prior to the return of the research residents, and a surgical education fellow and simulation center staff set up models in our simulation center including vascular anastomosis, hand-sewn and stapled bowel anastomosis, laparoscopic suturing, and a porcine trachea model for percutaneous tracheostomy. These are low-cost simulation models based on the ACS/APDS Phase 1 Curriculum, an "off-the-shelf" curriculum freely available to surgical training programs.11,12 A variety of expired surgical devices are also provided to the returning residents to refresh their knowledge and develop comfort in their use. These devices include open and laparoscopic GIA staplers, EEA staplers, TA staplers, endocatch bags, endostitch, as well as kits for central lines, percutaneous tracheostomy, percutaneous endoscopic gastrostomy, pneumothorax. Multiple sessions allow for spaced and repetitive practice, and the simulation setting allows for returning residents to regain familiarity with procedures and devices without the stress associated with the operating room environment during actual patient care. During the pilot year of this program, 80 percent (n=8) of the returning residents participated in these targeted simulation sessions. Excluding the one returning resident who was the surgical education fellow organizing the session, 100 percent of these individuals (n=7) completed evaluations of the simulation sessions. All of the participants agreed or strongly agreed that the sessions increased their confidence and ability in performing these advanced technical skills and that they anticipated incorporating what they learned during the practice session into patient care in the future. The sessions have been continued annually given its high perceived value to the returning residents.
Aside from technical and teaching skills, returning clinical residents meet with the program director and department chair to discuss reentry with a focus on team leadership. This topic is developmentally appropriate for the majority of our returning residents who reenter as a clinical PGY-4. Additionally, the returning residents meet with the associate program director who is assigned to mentor PGY-4 residents. The associate program director works with the PGY-4 class annually and has become familiar with the issues surrounding the return to clinical residency and can provide guidance regarding imminent fellowship applications for competitive subspecialties, such as pediatric surgery and surgical oncology. To ensure early identification of residents who may be struggling with the return to clinical residency, the associate program director hosts intermittent check ins with the class as a group as well as individually. Finally, our research residents have continued opportunities to engage in clinical care and/or operative training, including paid moonlighting opportunities, large animal research, and cadaver-based labs. A recent group of MGH research residents reported an average of 26.75 operations completed during their research period (n=8 residents, range 4–100 operations, median=13.5 operations). While we have not studied the benefits of moonlighting, one potential additional benefit beyond the operative exposure is the opportunity to remain up to date with hospital policy changes or shifts in clinical practice.
Many surgical trainees choose to interrupt their clinical training to pursue other professional interests such as research, global surgery, administration, or education. This practice is especially frequent at academic training programs that attract residents planning on pursuing careers in academic surgery. While this time is an investment in future career ambitions, there may be associated decline in clinical skills, particularly advanced technical skills and procedural knowledge. Unfortunately, there is limited research on how to best support residents returning to clinical residency. We have described a number of interventions surgical training programs could implement to intentionally support their returning residents both during their professional development time and just prior to their reentry to full-time clinical residency. Future research may illuminate the "best practices" for how to ensure successful transition of residents back to full-time patient care.