Abstract
Background
In 1735, Dr. Claudius Amyand performed the first documented appendectomy after a swallowed sewing needle surreptitiously made its way to its appendiceal resting place. Revisiting this exact circumstance is the case of a 17-year-old male who inadvertently swallowed a sewing needle, after which it became lodged within his appendix.
Summary
The patient presented in no acute distress following the accidental swallowing of a sharp object. While he exhibited some mild pain and cramping, he denied complaints of sharp epigastric, gastric, or abdominal pain. The needle was identified on chest X ray and was presumed to be in the stomach. Esophagogastroduodenoscopy was unsuccessful for visualization and possible retrieval, but a normal esophagus was noted. The foreign object's transit through the small bowel was followed through serial imaging over the next two days. At approximately 48 hours post presentation, the patient experienced novel right lower quadrant pain and a bloody bowel movement. After radiologic CT suggested intra-appendiceal entrapment of the foreign object, emergent laparoscopic appendectomy was performed. No perforation of the appendix was noted on visual or pathological inspection, and the patient was discharged with no further complications on postoperative day 1.
Conclusion
Presented here is a unique case of swallowed foreign object entrapment within the appendix, documented only 250 times previously in the literature. In contrast to the case's 285-year predecessor, there was no perforation of the appendix observed on examination. While the aspiration and inadvertent swallowing of foreign objects are common in young pediatric populations, it seldom necessitates emergent surgical intervention.
Key Words
Amyand hernia; appendiceal; appendix; intrathoracic foreign body
Abbreviations
CXR: chest X ray
KUB: kidney ureter bladder X ray
Case Description
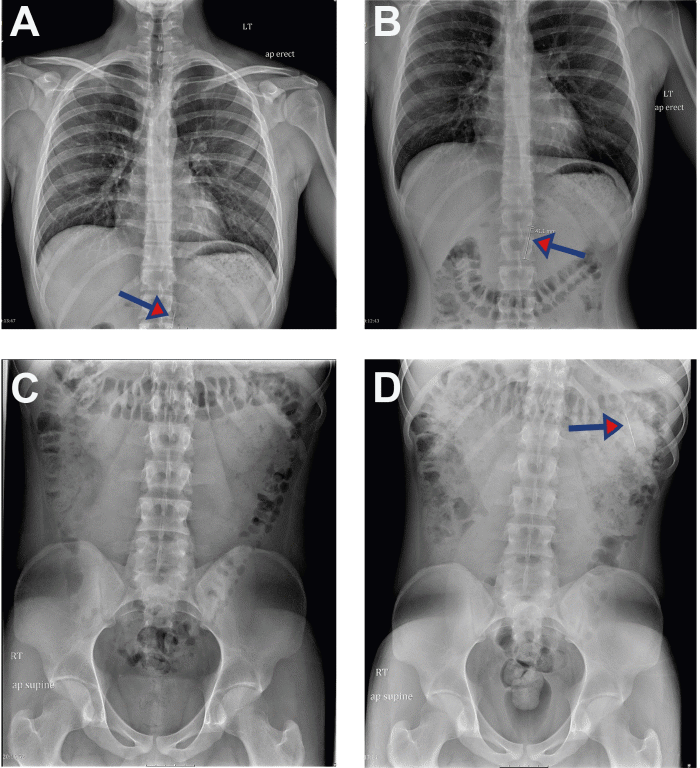
A 17-year-old male presented to the medicine service of the pediatric hospital after inadvertently swallowing a sewing needle while orally holding it in preparation to reset a phone. He exhibited some mild cramping but denied complaints of sharp epigastric, gastric, or abdominal pain. The needle was identified on chest (CXR) and kidney ureter bladder X-ray (KUB), presumably in the stomach or duodenum and measuring approximately 41 mm (Figure 1).
Esophagogastroduodenoscopy was performed, and while a small abrasion on the tongue was noted, the esophagus appeared normal, and the foreign object was not successfully visualized. CT imaging without contrast from the lung bases through the pelvis revealed a slightly distended stomach, normal bowel caliber with scattered fluid in the small bowel, as well as a normal appendix, and moderate stool and gas through the colon with no free air, fluid, or evidence of a visible foreign body (Figure 2).
Figure 1. CXR and KUB Demonstrating Needle Visualization and Transit Through Patient's Upper GI System Over Time. Published with Permission
Figure 2. Lack of Foreign Object Visualization on Initial CT. Published with Permission
Following the lack of foreign object visualization and retrieval, the patient was monitored with serial abdominal exams and X rays and was continued on polyethylene glycol 3350 to encourage passage of the sewing needle with bowel movements. Passage of the needle, possibly into the right ascending colon, was noted on CXR (Figure 3) approximately 48 hours after admission, with no evidence of bowel obstruction or pneumoperitoneum. Shortly after, however, the patient developed novel right lower quadrant pain and a bloody bowel movement. CT was indicated and revealed an elongated metallic density seemingly within the appendix (Figure 4), with no pericolonic appendiceal gas or fluid collection or noteworthy changes in lungs, liver, spleen, gallbladder, pancreas, adrenal glands, inferior vena cava, aorta, kidneys or bladder. The patient was referred for emergent laparoscopic appendectomy.
Figure 3. Sequential KUB Imaging Reveals Needle Transit Through Small Bowel. Published with Permission
Stat KUB was performed prior to surgery to verify foreign object location, and labs were within normal limits. A 5 mm incision was made in a curvilinear fashion at the superior umbilicus, and tissue was dissected down bluntly until the peritoneum was entered under direct vision. A 5 mm trocar was inserted, and direct visualization and pneumoperitoneum were obtained. Visualized bowel appeared viable and healthy, and there was no evidence of local inflammation in the area surrounding the appendix or free fluid present. A second 5 mm trocar was placed in the lower midline, and a third 12 mm trocar was placed in the left lower quadrant. When elevating the appendix, it appeared, upon palpation with a blunt instrument, that the foreign body was present in the mid appendix. A window was created between the base of the appendix and the mesoappendix using blunt dissection. The mesoappendix was divided, and no evidence of perforation or the sharp metallic foreign body within the lumen of the appendix was observed.
Figure 4. CT Demonstrated Evidence of Appendiceal Entrapment of Foreign Object. Published with Permission
The appendix was grasped at the distal tip and brought through the 12 mm trocar site. The foreign body was palpated in the mid appendix with no evidence of perforation, and the specimen was passed off for permanent pathology. A single piece of SURGICEL SNoW™ was used to stem oozing from where the mesoappendix was divided, and hemostasis was observed. Trocars were removed under direct visualization, and the pneumoperitoneum was evacuated. Wounds were copiously irrigated with normal saline, and deep dermal tissue was closed with 3-0 Vicryl™ followed by incision closure with 4-0 Monocryl™. Pathology report noted a 7.5 × 0.7 cm vermiform appendix containing a 3.7 cm silver straight pin with a 0.3 cm spherical pearl-like end toward the tip, which was located 1.5 cm from the tip of the appendix and lodged within the 0.3 cm lumen (Figure 4D). Sparse inflammation was noted. The patient recovered well from the procedure and returned home on postoperative day 1.
Discussion
Pediatric foreign body ingestion, intentionally or unintentionally, is a common occurrence in the United States, with more than 100,000 cases reported each year. Cases typically peak between 6 months to 3 years of age.1,2 While most objects pass without complication, an extremely rare percentage (0.0005%), as identified in a 100-year review of 256 cases, have been documented to find their way into the lumen of the appendix.3 While ingestion and entrapment of a straight pin in the appendix have only been documented a few times in the past 250 years, this exact situation prompted one of the first documented appendectomies by Dr. Claudius Amyand in 1735.4,5 Of the procedure on an 11-year-old male, Dr. Amyand writes, "View the Aperture made in it by the Pin hitherto concealed, through which that Part of it, which was incrusted with Chalk, had juft [sic] made its way out upon the an occafional Preffure [sic], as a Cork out of a Bottle."5 Perforation of the pin through the elongated appendix "greatly disturbed" Amyand due to the "discharge of feces coming out of the gut," prompting alteration to the surgical course and necessitating urgent removal of the damaged appendix. Following this case, the term Amyand's hernia was coined, referring to cases where the vermiform appendix herniates through the inguinal sac, as occurred in this patient. Amyand's hernia, occurring mostly in children due to the patency of the processus vaginalis, has an incidence reported between 0.19% and 1.7% of all hernias.6,7
In addition to Dr. Amyand's case, the only other two previously documented cases of straight pin ingestion were in 1886 and 2006. Previously, most cases of appendiceal object entrapment have caused signs of gross inflammation or perforation and have occurred in younger children. In the case described here, the teenaged patient's inadvertent swallowing resulted in appendiceal entrapment of the sharp foreign object without perforation, gross inflammation, or Amyand hernia formation.4,8
Accidental ingestion of foreign objects is common in the young pediatric population. Once objects are past the esophagus, 80-90% pass without complication in 3 to 7 days and can usually be followed by serial X rays as was initiated in this case prior to complication.9-11 In the minority of cases that result in complications, the overwhelming majority are limited to small bowel obstruction, perforation, or erosion into adjacent organs.2,12
In contrast, this case report highlights a unique circumstance in which an adolescent outside of the typical age range for foreign body ingestion experienced the unique complication of entrapment of the foreign object within the appendix, necessitating an emergency appendectomy. When specifically considering straight pins with a small head, a review from the early 1930s found that the majority were aspirated—with 63% of 113 cases lodging within the main or segmental bronchi—rather than swallowed.13 Interestingly, of the few objects which have been documented to lodge within the appendix, the majority are metallic objects such as drill bits, fishhooks, pins, bullets, and air gun pellets. When sharp, these objects also increase the risk of appendiceal perforation.3 Considering this risk and the patient's worsening clinical condition, the decision was made for an emergent laparoscopic appendectomy. Fortunately, there was no perforation of the appendix noted in this case.
Conclusion
While the impetus may have evolved over the centuries, from casually holding a pin in the mouth (prompting the first appendectomy in 1735) to resetting a cell phone today, the accidental swallowing of straight pins has persisted.5 In this case, the decision was made for an emergent laparoscopic appendectomy following an abrupt change in the patient's clinical condition, accompanied by radiologic evidence of possible entrapment of the swallowed foreign object in the appendiceal lumen. While this once-in-a-century occurrence has previously resulted in inflammation, perforation, and Amyand hernia formation in younger children, this unique case in a teenage child concluded without such complications.4
Lessons Learned
Aspiration of a sharp metal object in an adolescent teen resulted in the unique complication of entrapment within the appendiceal lumen. A low threshold for emergent appendectomy should be considered when appendiceal entrapment of a sharp foreign object is suspected to minimize the chance of perforation and further complications.
Authors
Spellicy SEa; Walker ESb; Holtzclaw LAc; Rowlett JDe
Author Affiliations
- University System of Georgia, Medical College of Georgia, Augusta, GA 30912
- Department of General Surgery, St. Joseph's Candler Hospital, Savannah, GA 31405
- Physician Assistant Program, Medical College of Georgia, Augusta, GA 30912
- Department of Pediatrics, Medical College of Georgia, Savannah, GA 31405
Corresponding Author
John D. Rowlett, MD, FAAP, FACP
6 Calico Crab Retreat
Savannah, GA 31411
Email: drrowlett@gmail.com
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: April 8, 2021
Accepted: July 13, 2021
References
- Wyllie R. Foreign bodies in the gastrointestinal tract. Curr Opin Pediatr. 2006;18(5):563-564. doi:10.1097/01.mop.0000245359.13949.1c
- Uyemura MC. Foreign body ingestion in children [published correction appears in Am Fam Physician. 2006 Apr 15;73(8):1332]. Am Fam Physician. 2005;72(2):287-291.
- Klingler PJ, Seelig MH, DeVault KR, et al. Ingested foreign bodies within the appendix: A 100-year review of the literature. Dig Dis. 1998;16(5):308-314. doi:10.1159/000016880
- Llullaku SS, Hyseni NSh, Kelmendi BZ, Jashari HJ, Hasani AS. A pin in appendix within Amyand's hernia in a six-years-old boy: case report and review of literature. World J Emerg Surg. 2010;5:14. Published 2010 May 19. doi:10.1186/1749-7922-5-14
- Amyand C. VIII. Of an inguinal rupture, with a pin in the appendix coeci, incrusted with stone; and some observations on wounds in the guts. Phil Trans R Soc. 1735;39(443):329-342. doi:10.1098/rstl.1735.0071
- Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR. Amyand's hernia: a review. Med Sci Monit. 2014;20:140-146. Published 2014 Jan 28. doi:10.12659/MSM.889873
- Cankorkmaz L, Ozer H, Guney C, Atalar MH, Arslan MS, Koyluoglu G. Amyand's hernia in the children: a single center experience. Surgery. 2010;147(1):140-143. doi:10.1016/j.surg.2009.09.038
- Hall RJ. Suppurative peritonitis due to ulceration and suppuration of the vermiform appendix; laparotomy; resection of the vermiform appendix; toilette of the peritonaeum; drainage; recovery. NY Med J. 1886;43:662-663
- Anderson KL, Dean AJ. Foreign bodies in the gastrointestinal tract and anorectal emergencies. Emerg Med Clin North Am. 2011;29(2):369-ix. doi:10.1016/j.emc.2011.01.009
- Alabkary S, Al-Buainain H, Elshafei H. Ingested metallic foreign body lodged within the appendix. J Pediatric Surgery Case Reports. 2018;32:39-40. doi:10.1016/j.epsc.2018.01.011
- Bekkerman M, Sachdev AH, Andrade J, Twersky Y, Iqbal S. Endoscopic Management of Foreign Bodies in the Gastrointestinal Tract: A Review of the Literature. Gastroenterol Res Pract. 2016;2016:8520767. doi:10.1155/2016/8520767
- Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001;160(8):468-472. doi:10.1007/s004310100788
- Jackson C, Jackson CL. Pins at the Periphery of the Lung: Observations Based on Forty-Two Cases. Arch Otolaryngol. 1932;15(6):860-882. doi:10.1001/archotol.1932.03570030882005