Abstract
Background
This case report describes the benefits of a novel technique to incise the skin. Most surgeons will use a cold scalpel for full-thickness skin incisions, which results in excess bleeding, then spend time achieving hemostasis with electrocautery. Alternatively, the use of electrocautery as the sole instrument to make full-thickness skin incisions causes thermal injury and poor cosmetic results. Likewise, extensive use of electrocautery on epidermal and dermal tissues produces surgical smoke, which, when inhaled, can cause long-term complications and has been shown to contain many known carcinogens. This technique utilizes the strengths of both modalities to create a better incision.
Summary
Scalpel incision is made superficially and lightly through the epidermal layer to avoid bleeding; subsequently, electrocautery set on 10-cutting is used to incise the dermis and hypodermis.
Conclusion
This is an improved incisional technique that may lead to better cosmesis, less thermal injury, and improved surgical workplace safety.
Key Words
electrocautery; Bovie; monopolar; incision; scalpel; surgical smoke
Case Description
When surgeons and patients evaluate their incisions, there is a consensus that the most important outcome after cutaneous wound repair is the presence of infection and cosmetic appearance.1 Wound infection has been directly linked to cutaneous trauma secondary to the destruction of the epidermal barrier, as evidenced by burn injury infection rates. Since the advent of William T. Bovie's electrosurgical device (i.e., electrocautery/diathermy/monopolar) and its push into the surgical theater by Dr. Harvey Cushing in 1926, continued attempts have been made to replace the scalpel with this newer technology to create an incision. While much of the research comparing these two modalities has focused on outcomes such as pain, bleeding, incision time, and infection rates, few have significantly considered the cosmetic differences.1-3 As a result, there remains debate on the specific incisional tool and technique utilized to begin what is essential to all surgeries, the incision. Most utilize a hybrid technique of incising skin with a scalpel and controlling skin bleeding with electrocautery (Figure 1). Unfortunately, while electrocautery aids in obtaining hemostasis, it often results in dermal and epidermal burn injury from beneath. We propose a novel technique to incise the skin that optimizes hemostasis and yet avoids epidermal thermal injury for maximal cosmesis.
Figure 1. Scalpel Incision of Epidermis and Dermis. Published with Permission
A.
Using a scalpel, the epidermal layer of the skin is split, exposing the white dermal layer (Figure 2A). What remains is the underlying dermal and hypodermal layers containing the skin's blood supply. Thus, there is little to no bleeding when only the epidermis is incised.
Using firm digital traction to the skin edges, separating the epidermal layer further, electrocautery set on 10-cutting (blend) is used to incise the dermis and hypodermis (Figure 2B). This produces just enough energy to incise the tissue without significant thermal injury as well as enough coagulation to seal the small blood vessels in the hypodermis. Having achieved a complete separation of the skin, any subcutaneous bleeding subsequently encountered during dissection can be cauterized using standard settings without inflicting thermal injury to the skin.
Figure 2. Scalpel Incision of Epidermis, Exposing Underlying White Dermis with Minimal Bleeding. Published with Permission
A.
Discussion
Using a scalpel to incise the skin is quick and minimally traumatic to the surrounding tissue. The vasculature of the skin, which is located in the hypodermis, is also disrupted, often leading to bleeding from the skin edge. This bleeding often requires additional measures to control hemostasis, using electrocautery. Unfortunately, electrocautery, usually used on a setting of 30-coagulation (blend), also results in thermal injury to the surrounding tissue.
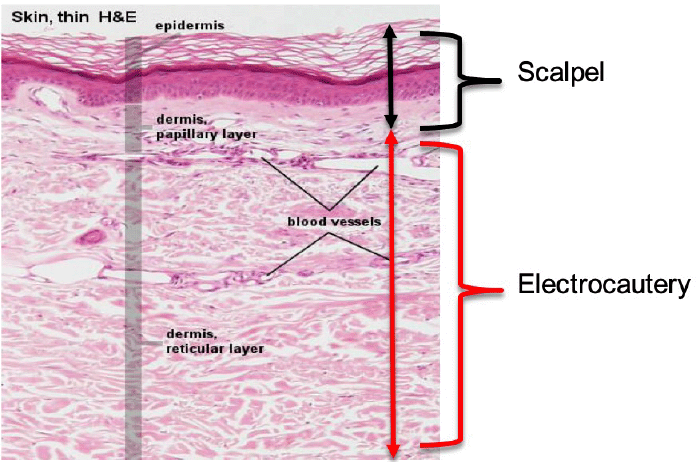
The science behind an ideal incision has principles that are often overlooked in histology. An incision using a scalpel avoids the lateralizing thermal trauma imposed on the relatively avascular epidermis, particularly the deepest epidermal layer, the stratum basale composed of stem cells. With this technique, the goal is transection of the epidermis down to the level of the papillary dermis just prior to the reticular dermis and subdermal layers below (Figure 3).4 The papillary layer is composed of loose connective tissue containing capillary projections that serve but do not enter the epidermis. As incision via scalpel lacks a hemostatic component, electrocautery is then used to complete the incision once the stem cells of the stratum basale are safeguarded.
Figure 3. H&E Histological Slide Demonstrating Layers of Skin (4). Published with Permission
Electrocautery technology converts the electricity of the main supply (240V; 50 Hz) into high-frequency current (>100,000 Hz), minimizing the risk of electrical shock.5 This concentrated current induces heat energy capable of a range of effects: from drying out cells—with consequent coagulation of blood, to vaporization of cells—permitting an electrode to physically separate tissue.6 This degree of current concentration is called "current density." The surface area the current is passed through determines the current density. Thus, the electrocautery pad (dispersive electrode) placed on the patient has a large surface area, reducing the current density.6 The pad creates a complete circuit through the patient, with the cutting cautery blade being the smallest surface area (highest current density), resulting in high resistance and heat energy.
There are two clinical modes of cautery: cut and coagulation. Cutting is further subdivided into pure cut and blended cut. In blended cut, some coagulation mode is added, producing a hemostatic effect. In pure cut, the cautery performs more as a knife with minimal hemostasis, and heat energy vaporizes cells.6 With blended cut, cooling periods slow down the action, replacing vaporization with slow dehydration of cellular fluid and protein, ideal for sealing off small bleeders.6
Tissue burns are divided into superficial, partial thickness, deep partial thickness, and full thickness burns. Normal classifications of thermal injury do not apply to electrocautery since all layers are involved, but the lateral extent of the thermal injury distinguishes healing. It can be assumed that the lower the energy used (current density), the lower the thermal injury. This should correlate with improved healing, but no formal studies have examined this.
Our technique uses a low-cutting electrocautery setting to complete the incision. With the cutting setting, a high-density sinusoidal current is focused over a small portion of tissue. Due to its resistive properties, it causes a rapid rise in temperature, vaporization, and subsequent separation of tissue along the incision line.7 When the subdermal tissue is encountered with its rich network of blood vessels, the coagulation portion of the blend mode produces a low current density spreading over a large area, not sufficient to reach vaporization but denaturing proteins forming a viscous coagulum that retards blood flow.7
Considering significant wound outcomes such as infection rates, Aird and Brown demonstrated via meta-analysis (n=1196) strong evidence for similar rates of wound infection when either a scalpel or electrocautery was used.2 Interestingly, Ahmad and Ahmed completed an additional meta-analysis (n=3122, 1627 scalpel and 1495 electrocautery) illustrating that postoperative pain was significantly less with electrocautery incisions in the first 24 hours.3 The authors noted that the painless nature of full-thickness burns could be attributed to the destruction of nerve endings when electrocautery is utilized. Unfortunately, cosmetic comparisons between the two have not been thoroughly evaluated because of a scarcity of available data, as mentioned in both meta-analyses.
The importance of our technique is not only rooted in outcomes that we strive for in our patients but also in reducing workplace risks and hazards to operating room personnel. Surgical smoke produced from electrocautery is an inescapable trade-off of functionality. Electrocautery produces particles ranging from 0.07 to 0.42 um. It is well known that particulate matter 10 um and smaller can be inhaled, causing irritation and long-term complications such as CAD, congestive heart failure, asthma, and COPD.8 Likewise, investigation of the specific composition of surgical smoke has identified many carcinogens. Cauterized epidermal tissue has been demonstrated to contain higher levels of toluene, ethylbenzene, and xylene compared to adipose tissue, which produces higher levels of aldehydes.8 For these reasons, limiting electrocautery to the low-cutting setting while on the remainder of the dermis and using higher-setting coagulation while on the subdermal tissue is beneficial to wound outcomes and safer.
Conclusion
We propose an improved incisional method that implements the best aspects of the scalpel and electrocautery based on electrophysiological and histological principles, resulting in better cosmesis, less thermal injury, reduced cutaneous bleeding, and improved surgical workplace safety.
Lessons Learned
An improved scalpel and electrocautery incisional technique that reduces cutaneous bleeding, produces better cosmesis, diminishes thermal injury, and improves surgical workplace safety.
Authors
Maldonado EJa; Trocha Ka; Lotakis Da; Wallack MKa; Finlay DJa,b
Author Affiliations
- Department of Surgery, Metropolitan Hospital Center at New York Medical College, New York, NY 10029
- Division of Vascular Surgery, Department of Surgery, The Mount Sinai Medical Center, New York, NY 10029
Corresponding Author
Eric J. Maldonado, MD
Metropolitan Hospital
1901 1st Avenue
New York, NY 10029
Email: maldonae8@nychhc.org
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: June 26, 2021
Accepted: December 6, 2021
References
- Singer AJ, Quinn JV, Thode HC Jr, Hollander JE; TraumaSeal Study Group. Determinants of poor outcome after laceration and surgical incision repair. Plast Reconstr Surg. 2002;110(2):429-437. doi:10.1097/00006534-200208000-00008
- Aird LN, Brown CJ. Systematic review and meta-analysis of electrocautery versus scalpel for surgical skin incisions. Am J Surg. 2012;204(2):216-221. doi:10.1016/j.amjsurg.2011.09.032
- Ahmad NZ, Ahmed A. Meta-analysis of the effectiveness of surgical scalpel or diathermy in making abdominal skin incisions. Ann Surg. 2011;253(1):8-13. doi:10.1097/SLA.0b013e3181ff461f
- Slomianka L. Blue histology - integumentary system. University of Western Australia-School of Anatomy and Human Biology. http://lecannabiculteur.free.fr/SITES/UNIV%20W.AUSTRALIA/mb140/CorePages/Integumentary/Integum.htm. Published April 26, 2000. Accessed October 5, 2019.
- Saaiq M, Zaib S, Ahmad S. Electrocautery burns: experience with three cases and review of literature. Ann Burns Fire Disasters. 2012;25(4):203-206.
- McCauley G. Understanding Electrosurgery. Bovie Medical Corporation. Clearwater, FL., MC-55-049-001. Rev.2.
- O'Connor JL, Bloom DA. William T. Bovie and electrosurgery. Surgery. 1996;119(4):390-396. doi:10.1016/s0039-6060(96)80137-1
- Limchantra IV, Fong Y, Melstrom KA. Surgical Smoke Exposure in Operating Room Personnel: A Review. JAMA Surg. 2019;154(10):960-967. doi:10.1001/jamasurg.2019.2515