Abstract
Background
Inferior vena cava obstruction in patients with end-stage renal disease constitutes a relative contraindication to renal transplantation. We report a case of both superior vena cava (SVC) and inferior vena cava (IVC) obstruction receiving a successful renal transplant from a deceased donor.
Summary
The recipient is a 23-years old male with CKD secondary to nephrotic syndrome who also had antiphospholipid syndrome and had been on long-term anticoagulation. The transplant was achieved by anastomosing the renal vein to the patent external iliac vein, which was shown to drain through a complex collateral system. At one year, the patient had a serum creatinine of 136 umol/L and an estimated GFR of 56 mL/min.
Conclusion
Most cases of pelvic vein or IVC thrombosis in patients with CKD is provoked by the insertion of a dialysis line. It is widely recommended that a femoral line for dialysis should only be used in an emergency when no other access is available. It should be for the shortest possible duration until more suitable access (e.g., an arteriovenous fistula or a transplant) is achieved.
Key Words
renal transplant; inferior vena cava; thrombosis; outcome
Abbreviations
CKD: chronic kidney disease
IVC: inferior vena cava
SVC: superior vena cava
CIV: common iliac vein
EIV: external iliac vein
IIV: internal Iliac vein
PV: portal vein
SMV: superior mesenteric vein
eGFR: estimated glomerular filtration rate
Case Description
The patient was a 23-year-old male with chronic kidney disease (CKD) secondary to nephrotic syndrome. He had been on hemodialysis for 12 years, more recently, through a left arteriovenous fistula (AVF). He had a history of bilateral neck and femoral line insertion for dialysis. The patient had both SVC and IVC obstruction with facial swelling and extensive collateral veins on the anterior abdominal and chest walls. He had undergone angioplasty of the neck and pelvic veins with recurrent stenoses. The patient also had antiphospholipid syndrome (APS) and has been on long-term anticoagulation. The patient had been deemed unsuitable for transplant at his local transplant center. A CT angiogram revealed occlusion of the right external iliac (EIV), right common iliac (CIV), and the entire length of IVC. Both renal veins were also occluded. The left EIV and CIV were patent with occlusion of CIV at its junction with the IVC. The proximal left CIV drained through the right internal iliac vein and ascending lumbar vein and also right femoral vein.
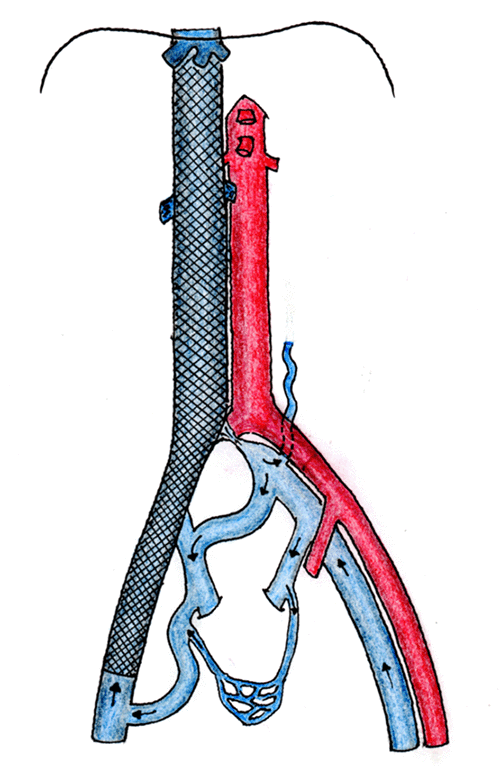
Prior to his transplant, the patient underwent recanalization of the right EIV, right CIV, and the IVC up to the hepatic veins with multiple self-expanding stents (Figure 1). The IVC recanalization was achieved by establishing the right common femoral vein access under ultrasound guidance and negotiating a catheter-supported straight-tipped hydrophilic wire across the length of the iliac vein and the occluded IVC under fluoroscopic guidance. The successful crossing of the occlusion was confirmed with contrast injection into the right atrium. The length of the occlusion was initially balloon dilated and then supported with large caliber self-expanding stents, two for the IVC and one for the CIV and EIV. Postprocedure fluoroscopy demonstrated a good flow of contrast through the IVC and into the right atrium. Venous pressures were not measured in this procedure.
Figure 1. CT Abdomen Angiogram with Author Rendering. Published with Permission
The patient underwent a kidney transplant from a seven-year-old female brain stem dead donor who had died of cardiac arrest secondary to hypertrophic cardiomyopathy. The donor's right kidney had normal anatomy with a single renal artery, vein, and ureter. The HLA mismatch was 2A, 2B, and 2DR (i.e., a complete mismatch). The transplant was carried out in the left iliac fossa. Care was taken not to cut through any significant collateral veins. The venous pressure in the external iliac vein was 12.5 mm Hg (17 Cm H2O). The pressure in the vein was measured by inserting a green (21 g) needle into the EIV and connecting this through plastic tubing to a pressure transducer. The renal vein was anastomosed to EIV, and the renal artery to the external iliac artery. The reperfusion was slow and suboptimal, with good flow through the renal artery and no evidence of venous hypertension. The anastomosis time was 41 minutes, and the cold ischemic time was 9 hours and 10 minutes. Intravenous bolus heparin 1000 IU was administered before clamping the iliac vessels.
The patient initially had slow graft function and required one dialysis session on day 3 for hyperkalemia. Graft function gradually improved from day 6, and the patient was discharged home on day 16 with steadily improving serum creatinine of 328 umol/L. Improvement in graft function correlated with the Doppler findings with initially poor cortical flow and subsequently improved flow as function started to improve.
The immunosuppression induction was with antithymocyte globulin (ATG, Rabbit-Fresenius), starting intraoperatively and continuing for five days after the transplant. The maintenance immunosuppression included tacrolimus, Cellcept, and prednisolone. A trough level of tacrolimus was aimed at 9–15 ng/mL in the first three months. Antibiotic, antifungal, and antiviral prophylaxis were started according to the transplant unit protocol. Given the history of recurrent thrombosis and familial coagulopathy, the patient was commenced on intravenous heparin on day 0, converting to a therapeutic dose of enoxaparin once the transplant was stabilized.
Two months after the transplant, the patient presented with deteriorating graft function and hypertension. Postanastomotic renal artery stenosis was successfully treated with angioplasty and stent insertion, with subsequent improvement in graft function and blood pressure control. At one year, the patient had a serum creatinine of 136 umol/L and an estimated GFR of 56 mL/min.
Discussion
Renal transplant is the best treatment for end-stage renal disease with associated improved quality of life and overall survival compared to chronic dialysis.1 Often, a transplant is not possible due to recipient-related factors. Active malignancy, a history of certain types of malignancies, and debilitating cardiorespiratory illness are absolute contraindications to transplantation. Anatomical problems such as lack of space, suitable vascular inflow and outflow, and lower urinary tract problems often pose difficult challenges and may render transplant impossible.
All recipients of renal transplants are assessed for surgical suitability concerning vascular inflow, outflow, and appropriate urinary drainage. Any intervention for a correctable anomaly of the inflow, outflow, or lower urinary tract should be undertaken prior to the transplant. Unobstructed low-pressure venous drainage is the key to the success of transplant. Conventionally transplants are performed in the pelvis with vascular anastomoses to the iliac vessels. Hence any obstruction in the venous system cranial to the site of anastomosis in the absence of satisfactory collateral drainage will result in venous hypertension, likely renal vein thrombosis, and graft failure.
Thrombosis or stenosis of the IVC poses a unique challenge making transplant impossible in either iliac fossa. The feasibility of recanalizing the IVC through vascular intervention should be considered in these cases. Occasionally, a transplant will be possible without recanalization of the IVC. A thorough search for collateral drainage should be undertaken with a CT or MR angiogram aiming to transplant onto the collaterals or to a patent distal vein drained by these collaterals. The collateral veins in the presence of IVC thrombosis are thin-walled and are likely to have high venous pressure making transplant technically challenging and with an increased risk of renal vein thrombosis. When using a collateral vein or a pelvic vein distal to the obstruction, it is important to rule out venous hypertension. The normal pressure range in the pelvic veins and IVC range is 0–15 mm Hg and vary in accordance with intraabdominal pressure.2-4 Persistent venous hypertension in the renal vein and in the draining vein indicates inadequate drainage and is a risk factor for renal vein thrombosis after renal transplant.5,6 In cases where the IVC thrombosis is distal to the renal veins, transplant can be considered onto a sufficiently dilated left gonadal vein or, in an orthotopic position, onto the patent renal vein.7,8
In cases where IVC recanalization is not possible, and sufficient low-pressure collaterals are not established, renal vein outflow through a portal venous system may be considered. Successful transplants have been achieved by utilizing portal, splenic, superior mesenteric, and inferior mesenteric veins as outflow for the transplanted kidney.9-12 It must be stressed that transplantation onto PV and SMV carries a high risk and should only be attempted as a last resort in an experienced center and with informed consent.
Aikawa et al. have shown anastomosis of the renal vein to the azygos vein, IVC (above the obstruction), and the portal vein in a case series of pediatric recipients with IVC obstruction.13 Other authors have reported successful transplants with venous outflow to gonadal,7 inferior mesenteric,12,14 and collateral veins.15 Seiichiro and colleagues, in their review of 11 cases of pediatric transplants, have reported venous anastomoses to suprarenal IVC, left renal vein, and ascending lumbar vein. They also report additional venous anastomosis to the splenic vein in two cases where pressure in the renal vein was found to be high after the transplant.16 Verghese et al. have reported venous drainage to the right hepatic vein using a venous conduit in pediatric recipients.17
The insertion of a dialysis line provokes most cases of pelvic vein or IVC thrombosis in patients with CKD. It is widely recommended that a femoral line for dialysis should only be used in an emergency when no other access is available. It should be for the shortest possible duration until more suitable access, e.g., an arteriovenous fistula or a transplant, is achieved. In a small number of cases, the patients may have underlying coagulopathy resulting in extensive, often recurrent thrombosis.18 Protein-losing nephropathy (nephrotic syndrome) is often associated with coagulopathy and venous thrombosis.19,20 Familial coagulopathy, such as Factor V Leiden deficiency, antiphospholipid syndrome, and protein S deficiency, may also be associated with recurrent thrombosis and venous occlusion.15,21 All CKD patients with thrombosis and venous occlusion should, therefore, be screened for coagulopathy. Patients with familial coagulopathy should be managed with life-long anticoagulation.
A successful kidney transplantation requires an adequate arterial inflow and a low-pressure unimpeded venous drainage. Transplantation in the presence of IVC thrombosis poses a major challenge for transplant surgeons. Our patient had both SVC and IVC thrombosis and also had familial coagulopathy requiring life-long anticoagulation. The IVC occlusion involved the entire length of IVC, including the retrohepatic part. Both renal veins were small and thrombosed. Hence, no part of the IVC, renal, or gonadal veins was available for implantation. The right EIV, CIV, and distal left CIV were also occluded. While the left EIV and proximal CIV were patent, the left CIV at its junction with the IVC was occluded, precluding implantation onto these veins. A decision was therefore made to recanalize the IVC the right EIV, CIV through vascular intervention.
While recanalization of right EIV, CIV, and IVC restored the venous flow, implantation was technically impossible on the recanalized segments due to the metal stent. The postintervention image showed that the left CIV drained freely through the right internal iliac vein, the right EIV through pelvic collaterals, and the left ascending lumbar to the hemiazygos system. Therefore, implantation to the left external iliac vein was planned pending the absence of significant venous hypertension intraoperatively. The patient was fully informed of the complexity, including the possibility of being unable to transplant or early graft loss due to thrombosis. Implantation was successfully performed to the left EIV after the venous pressure was within the acceptable range.
Lonze et al. have described three cases with IVC and bilateral iliac vein thrombosis where the venous anastomosis was performed to the portal venous system in two cases and to the native left renal vein in the third. Arterial anastomosis was done to the aorta and common iliac and splenic arteries.21 Implantation to RV or left gonadal vein was impossible in our patient because of complete IVC and renal vein occlusion. We also considered venous outflow to the portal venous system as a last resort. However, given the patient history of recurrent thrombosis, this was considered high-risk and only a last resort. Implantation onto the right hepatic vein was also considered with the help of venous and arterial conduit as described by Verghese et al.16 This was also deemed high risk and was not required.
Our patient had a history of recurrent thrombosis of dialysis lines in the neck and femoral veins despite being on systemic anticoagulation and had developed both SVC and IVC occlusion. His thrombophilia may have been amplified by the combination of nephrotic syndrome, antiphospholipid syndrome, and insertion of multiple dialysis lines resulting in extensive large vein thrombosis involving both SVC and IVC. He had been deemed unsuitable for transplantation in the local center, had been on dialysis for ten years, and had precarious venous access for dialysis. A hypercoagulable state in renal transplant recipients is associated with inferior graft survival but does not constitute an absolute contraindication to renal transplant.
Our case exemplifies a unique combination of complete IVC thrombosis and familial thrombophilia initially deemed non-transplantable. We have demonstrated that a successful renal transplant is possible in such patients with a multidisciplinary approach and with careful planning and intervention. We suggest these transplants be performed in centers with an experienced multidisciplinary team.
Conclusion
IVC thrombosis constitutes a relative contraindication to renal transplantation. In this report, we have shown that with careful workup and planned intervention in a multidisciplinary setting, a successful kidney transplant is possible in the presence of complete IVC occlusion and associated coagulopathy.
Lessons Learned
It is imperative to investigate all patients with a history of recurrent thrombosis for underlying coagulopathy. With a thorough pre-transplant workup, use of systemic anticoagulation, and close posttransplant surveillance, satisfactory medium, and long-term graft survival can be achieved in these patients.22,23
Author Contribution
NA suggested the case report be written. LM collated the patient data and wrote the manuscript. NA reviewed and edited the initial manuscript. All authors reviewed and edited the final manuscript. NA edited and approved the final manuscript.
Authors
Moshref LHa; Abd Hammad MRa; Jameel Ma; Zia Zb; Ashour MAb; Habhab WTc; Ahmad Na
Author Affiliations
- Department of Surgery, Section of Transplantation, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia
- Department of Diagnostic and Interventional Radiology, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia
- Department of Medicine, Section of Nephrology, King Faisal Specialist Hospital and Research Centre, Jeddah, Saudi Arabia
Corresponding Author
Niaz Ahmad, MD, FRCS
Department of Surgery
Section of Transplantation & HPB Surgery
King Faisal Specialist Hospital and Research Centre
PO Box 40047 (J40)
Jeddah 21499
Saudi Arabia
Email: niazahmad@kfshrc.edu.sa
Disclosure Statement
The authors have no conflicts of interest to disclose. The Institutional Review Board (IRB) has also approved the case report at King Faisal Specialist Hospital and Research Centre, Jeddah, for publication. Approval Number: IRB 2021-CR-01
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: April 26, 2021
Revision received: August 15, 2021
Accepted: August 19, 2021
References
- Bailey P, Edwards A, Courtney AE. Living kidney donation. BMJ. 2016;354:i4746. Published 2016 Sep 14. doi:10.1136/bmj.i4746
- Markou N, Grigorakos L, Myrianthefs P, et al. Venous pressure measurements in the superior and inferior vena cava: the influence of intra-abdominal pressure. Hepatogastroenterology. 2004;51(55):51-55.
- Yung M, Butt W. Inferior vena cava pressure as an estimate of central venous pressure. J Paediatr Child Health. 1995;31(5):399-402. doi:10.1111/j.1440-1754.1995.tb00846.x
- Joynt GM, Gomersall CD, Buckley TA, Oh TE, Young RJ, Freebairn RC. Comparison of intrathoracic and intra-abdominal measurements of central venous pressure. Lancet. 1996;347(9009):1155-1157. doi:10.1016/s0140-6736(96)90611-x
- McArthur TA, Lockhart ME, Robbin ML. High venous pressure in the main renal vein causing development of peritransplant venous collaterals in renal transplant patients: a rare finding. J Ultrasound Med. 2011;30(12):1731-1737. doi:10.7863/jum.2011.30.12.1731
- Salvatierra O Jr, Concepcion W, Sarwal MM. Renal transplantation in children with thrombosis of the inferior vena cava requires careful assessment and planning. Pediatr Nephrol. 2008;23(12):2107-2109. doi:10.1007/s00467-008-0951-6
- Wong VK, Baker R, Patel J, Menon K, Ahmad N. Renal transplantation to the ovarian vein: a case report. Am J Transplant. 2008;8(5):1064-1066. doi:10.1111/j.1600-6143.2008.02185.x
- Mozes MF, Kjellstrand CM, Simmons RL, Najarian JS. Orthotopic renal homotransplantation in a patient with thrombosis of the inferior vena cava. Am J Surg. 1976;131(5):633-636. doi:10.1016/0002-9610(76)90032-5
- Rosenthal JT, Loo RK. Portal venous drainage for cadaveric renal transplantation. J Urol. 1990;144(4):969-971. doi:10.1016/s0022-5347(17)39635-0
- Rizzello A, Smyth O, Patel N, Reddy S, Sinha S, Vaidya A. Successful splenic venous drainage for kidney transplant in case of inferior vena cava thrombosis. Transplantation. 2011;92(10):e59-e60. doi:10.1097/TP.0b013e3182352d86
- Aguirrezabalaga J, Novas S, Veiga F, et al. Renal transplantation with venous drainage through the superior mesenteric vein in cases of thrombosis of the inferior vena cava. Transplantation. 2002;74(3):413-415. doi:10.1097/00007890-200208150-00022
- Patel P, Krishnamurthi V. Successful use of the inferior mesenteric vein for renal transplantation. Am J Transplant. 2003;3(8):1040-1042. doi:10.1034/j.1600-6143.2003.00177.x
- Aikawa A, Muramatsu M, Takahashi Y, et al. Surgical Challenge in Pediatric Kidney Transplant Vascular Anastomosis. Exp Clin Transplant. 2018;16 Suppl 1(Suppl 1):14-19. doi:10.6002/ect.TOND-TDTD2017.L41
- Patel P, Krishnamurthi V. Successful use of the inferior mesenteric vein for renal transplantation. Am J Transplant. 2003;3(8):1040-1042. doi:10.1034/j.1600-6143.2003.00177.x
- Lugo-Baruqui JA, Velásquez CA, Chen LJ, Ciancio G, Burke GW. Renal Transplantation in a Patient With Unsuspected Inferior Vena Cava Obliteration. Transplantation. 2016;100(10):2230-2233. doi:10.1097/TP.0000000000001039
- Shishido S, Kawamura T, Hamasaki Y, et al. Successful Kidney Transplantation in Children With a Compromised Inferior Vena Cava. Transplant Direct. 2016;2(6):e82. Published 2016 May 23. doi:10.1097/TXD.0000000000000592
- Verghese P, Minja E, Kirchner V, Chavers B, Matas A, Chinnakotla S. Successful Renal Transplantation in Small Children With a Completely Thrombosed Inferior Vena Cava. Am J Transplant. 2017;17(6):1670-1673. doi:10.1111/ajt.14213
- Gunawansa N, Sharma A, Halawa AM. Use of superior mesenteric vein for renal transplant venous outflow in a patient with extensive inferior vena cava thrombosis. World J Surg Surgical Res. 2018;1:1032.
- Mahmoodi BK, ten Kate MK, Waanders F, et al. High absolute risks and predictors of venous and arterial thromboembolic events in patients with nephrotic syndrome: results from a large retrospective cohort study. Circulation. 2008;117(2):224-230. doi:10.1161/CIRCULATIONAHA.107.716951
- Radhakrishnan J. Hypercoagulability in nephrotic syndrome. Uptodate. Last accessed 20 April 2020.
- Lonze BE, Dagher NN, Alachkar N, Jackson AM, Montgomery RA. Nontraditional sites for vascular anastomoses to enable kidney transplantation in patients with major systemic venous thromboses. Clin Transplant. 2017;31(12):10.1111/ctr.13127. doi:10.1111/ctr.13127
- Irish A. Hypercoagulability in renal transplant recipients. Identifying patients at risk of renal allograft thrombosis and evaluating strategies for prevention. Am J Cardiovasc Drugs. 2004;4(3):139-149. doi:10.2165/00129784-200404030-00001
- Heidenreich S, Junker R, Wolters H, et al. Outcome of kidney transplantation in patients with inherited thrombophilia: data of a prospective study. J Am Soc Nephrol. 2003;14(1):234-239. doi:10.1097/01.asn.0000039567.22063.9d