Abstract
Background
A young female patient presented with bilateral breast fibromatosis treated with bilateral mastectomy followed by one year of observation before planned reconstruction.
Summary
Our patient presented at age 20 with bilateral breast pain and retroareolar masses. Workup demonstrated bilateral breast fibromatosis with the involvement of large portions of both breasts. After failed symptomatic control with medical management, the patient underwent a bilateral skin-sparing mastectomy with plans for delayed reconstruction. No additional adjuvant therapies were required. She is being monitored closely for locally recurrent disease.
Conclusion
Despite benign pathology, patients may become symptomatic from breast fibromatosis, prompting surgical intervention. Given the high rate of local recurrence, surgical excision with wide margins is the recommended treatment of choice. However, radiotherapy has also been demonstrated to have good treatment efficacy. Hormonal therapy may also play a role in preventing progression or recurrence. The ideal management strategy for preventing local recurrence has not yet been established. As a result, the treatment of breast fibromatosis continues to pose a challenge. Patient factors such as age and extent of disease must be considered when tailoring a treatment regimen.
Key Words
breast fibromatosis; extraabdominal desmoid tumor
Case Description
A 20-year-old female with no prior history of breast mass or malignancy presented to our clinic after two years of progressive right-sided mastodynia with a corresponding palpable mass and associated retraction of her right nipple-areolar complex (NAC). She denied discharge or overlying skin changes. On exam, tender, ill-defined dense breast tissue was palpable posterior to the NAC with nipple inversion. Ultrasound revealed an indistinct mass-like enlargement of the right retroareolar breast (Figure 1A). Biopsy revealed low-grade spindle cell proliferation. The patient did not desire surgery at this time and was managed nonoperatively with oral analgesia and supportive clothing for symptom management.
Approximately one year later, the patient returned with worsening bilateral breast pain and a new rapidly enlarging left breast mass. On exam, the inversion of her left NAC was similar to the right. The right-sided mass had increased with gross distortion of normal breast architecture. Ultrasound imaging and biopsy of the left retroareolar mass were also consistent with breast fibromatosis. (Figure 1B). MRI imaging of both breasts demonstrated progressive enhancement kinetics of the bilateral masses with non-enhancing cores consistent with fibrosis/fibrotic tissue (Figure 1C and Figure 1D). Neither tumor had involvement of the overlying skin or the chest wall.
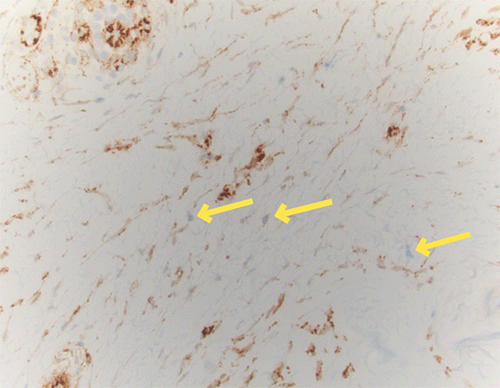
The patient underwent an uncomplicated skin-sparing bilateral mastectomy. Dense, fibrous breast tissue extending to the borders of the breast and down to the pectoral fascia was noted intraoperatively. Two large masses encased in breast tissue were completely removed (Figure 1E and Figure 1F). Histology revealed fascicles of bland spindle cells infiltrating normal ducts and lobules (Figure 2A, Figure 2B and Figure 2C). The spindle cells were positive for smooth muscle actin by immunohistochemistry but demonstrated only cytoplasmic positivity of beta-catenin (Figure 2D). The diagnosis of bilateral breast fibromatosis was rendered. The patient will be monitored closely for recurrence for 12 months before proceeding with breast reconstruction with tissue expanders.
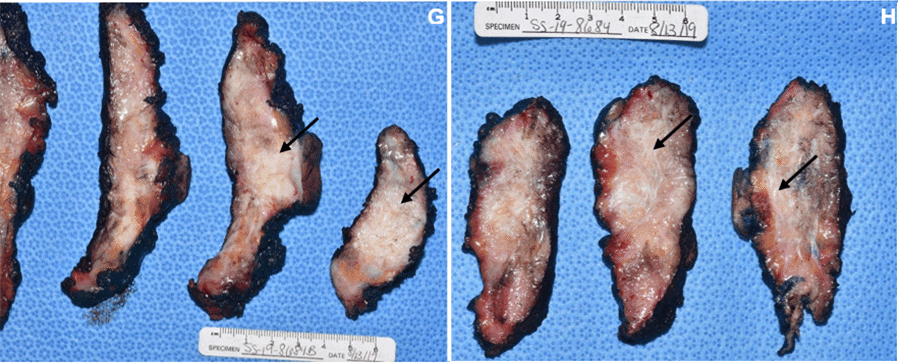
Figure 1. Ultrasound of Breast Mass and Excised Pathologic Specimen. Published with Permission
Figure 2. Histologic Sections of Specimen. Published with Permission
Discussion
Desmoid-type fibromatosis is a poorly circumscribed mesenchymal neoplasm typically arising from fibroblastic and myofibroblastic tissue. These tumors have aggressive growth patterns with invasion into the surrounding soft tissue but do not have metastatic potential.1-3 Due to local infiltration, recurrence rates are high after surgical excision, particularly in cases with inadequate margins.3 The estimated five-year cumulative risk of local recurrence of fibromatosis ranges from 17%–30%, with a greater risk of recurrence for fibromatosis of the extremities than those of the trunk.3,4,12,13
Grossly, fibromatoses resemble scar tissue with a tan-grey to white coarsely trabeculated surface on pathologic section (Figure 1G and Figure 1H). Histologically, a few differentiating features between desmoid tumors arising intra-abdominally and those arising in extra-abdominal regions can be appreciated.4 Typical histology reveals fascicles of spindle cells that insinuate between normal in situ structures. The cellularity of the lesion is variable, and the collagenous stroma ranges from indistinct to prominent. The spindle cells are bland with minimal hyperchromasia or atypia. Mitoses are rare.1,2,18 The immunophenotype of these spindle cells includes variable positivity for smooth muscle actin (SMA) and is commonly negative for desmin and CD34 phosphoglycoprotein. Notably, up to 80% of fibromatosis cases demonstrate aberrant nuclear localization of beta-catenin, which was not observed in this patient.18,19
Extra-abdominal desmoid tumors (EADTs) of the breast, known as breast fibromatosis, are a rare manifestation of this type of neoplasm. EADTs often present as a firm, tender mass first, with exam features concerning for carcinoma—approximately 14–20% of patients with breast fibromatosis present with skin dimpling or nipple retraction.3,4,7 More atypical presentations, such as dyspnea and ipsilateral upper extremity lymphedema, are secondary to advanced local invasion and the resulting mass effect.8,9 The vast majority of patients with breast fibromatosis are women; however, there are rare cases of men with breast fibromatosis documented.4,7 While the initial age of presentation is commonly between 30–50 years, some cases have been reported to be as young as 14 years up through 80 years of age.3,4,7,10
Due to the rarity of breast fibromatosis compared to other neoplasms of the breast, it is difficult to characterize its true incidence accurately. Aggregate data from several case studies and series have estimated breast fibromatosis to represent only 0.2% of primary breast lesions.3-6 The reported incidence of bilateral lesions is all the more exceedingly rare, making up only 4% of reported breast fibromatosis.6
The management of desmoid tumors remains a challenge nearly two centuries after John MacFarlane described it in 1832.16 Desmoid tumors are initially managed nonoperatively with serial imaging and oral medications, such as NSAIDs, if presenting symptoms do not necessitate surgical excision. If symptoms are intolerable and serial imaging demonstrates progressive growth threatening surrounding structures, a multidisciplinary approach is frequently needed, including surgical oncologists, radiation oncologists, and medical oncologists.12 Surgical resection with wide margins remains the standard management for desmoid tumors,2,3,6,7 but radiotherapy and hormone therapy have been successfully employed as alternatives.12,14,17 Controversy remains regarding which single modality or combination of modalities is most effective for treating this condition. Classically, re-excision for positive margins was regarded as necessary.2-4,10 In one of the largest meta-analyses of EADTs to date, the risk of local recurrence is almost twice as high in cases of positive margins.15 However, recent findings have questioned excisional margin status as an important prognostic indicator for risk of local recurrence, especially in cases where the adequacy of margins would result in significant morbidity.13 Radiotherapy alone has been shown to have similar efficacy to surgical resection in preventing local recurrence,12 and has positive modulatory effects as adjuvant therapy in cases of excision with positive margins.15 However, the data supporting surgical excision with adjuvant radiotherapy as a standard of care for the management of EADTs is still inconsistent.15,17
When arranging the treatment and care for the patient reported here, much consideration was given to her age at the time of presentation. Age less than 30 years is one of the significant patient factors correlated with poor control of local recurrence.12 The balance between the benefits of aggressive intervention and sparing a young patient desiring breast reconstruction from chest wall irradiation is not easily realized. Additionally, less toxic hormonal therapies, with agents like tamoxifen, have not been shown to have consistent clinical efficacy.5,14,17 Further prospective studies are greatly needed to establish a gold standard of treatment for EADTs of the breast. However, the sheer rarity makes adequate recruitment difficult. Presently, treatment decisions are made based on prior accounts of the successes and failures in treating breast fibromatosis and classic desmoid tumors.
Conclusion
Breast fibromatosis is a very rare entity in the general population with variable clinical presentation and progression. Wide local excision is recommended at the time of diagnosis. However, a standard of care for controlling long-term local recurrence has not yet been established. The balance of the risk and benefits should be individualized to minimize local recurrence and limit patient morbidity.
Lessons Learned
The current management of breast fibromatosis requires consideration of multiple patient factors when coordinating treatment.
Authors
Fang Ja; Bowie Ja; Barrena BGb; Chan ADa
Author Affiliations
- Department of Surgery, Naval Medical Center San Diego, San Diego, CA 92134
- Department of Pathology, Naval Medical Center San Diego, San Diego, CA 92134
Corresponding Author
Arden D. Chan, MD, FACS
General Surgery Department, NMCSD
34800 Bob Wilson Drive, Bldg 3-4
San Diego, CA 92134
Email: arden.chan1.mil@mail.mil
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: October 19, 2019
Revision received: February 10, 2021
Accepted: February 19, 2021
References
- Christopher DM, Bridge JA, Hogendoorn, Mertens F. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: International Agency for Research on Cancer; 2013
- Schnitt SJ, Connolly JL. Pathology of benign breast disorders. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the breast. 2nd ed. Philadelphia (PA): Lippincott Williams & Wilkins Publishers; 2000
- Wargotz ES, Norris HJ, Austin RM, Enzinger FM. Fibromatosis of the breast. A clinical and pathological study of 28 cases. Am J Surg Pathol. 1987;11(1):38-45. doi:10.1097/00000478-198701000-00005
- Rosen PP, Ernsberger D. Mammary fibromatosis. A benign spindle-cell tumor with significant risk for local recurrence. Cancer. 1989;63(7):1363-1369. doi:10.1002/1097-0142(19890401)63:7<1363::aid-cncr2820630722>3.0.co;2-b
- Taylor TV, Sosa J. Bilateral breast fibromatosis: case report and review of the literature. J Surg Educ. 2011;68(4):320-325. doi:10.1016/j.jsurg.2011.02.001
- Schwarz GS, Drotman M, Rosenblatt R, Milner L, Shamonki J, Osborne MP. Fibromatosis of the breast: case report and current concepts in the management of an uncommon lesion. Breast J. 2006;12(1):66-71. doi:10.1111/j.1075-122X.2006.00187.x
- Neuman HB, Brogi E, Ebrahim A, Brennan MF, Van Zee KJ. Desmoid tumors (fibromatoses) of the breast: a 25-year experience. Ann Surg Oncol. 2008;15(1):274-280. doi:10.1245/s10434-007-9580-8
- Schiller VL, Arndt RD, Brenner RJ. Aggressive fibromatosis of the chest associated with a silicone breast implant. Chest. 1995;108(5):1466-1468. doi:10.1378/chest.108.5.1466
- Glazebrook KN, Reynolds CA. Mammary fibromatosis. AJR Am J Roentgenol. 2009;193(3):856-860. doi:10.2214/AJR.08.1892
- Lee JC, Thomas JM, Phillips S, Fisher C, Moskovic E. Aggressive fibromatosis: MRI features with pathologic correlation. AJR Am J Roentgenol. 2006;186(1):247-254. doi:10.2214/AJR.04.1674
- Bishop AJ, Zarzour MA, Ratan R, et al. Long-Term Outcomes for Patients With Desmoid Fibromatosis Treated With Radiation Therapy: A 10-Year Update and Re-evaluation of the Role of Radiation Therapy for Younger Patients. Int J Radiat Oncol Biol Phys. 2019;103(5):1167-1174. doi:10.1016/j.ijrobp.2018.12.012
- van Broekhoven DL, Verhoef C, Elias SG, et al. Local recurrence after surgery for primary extra-abdominal desmoid-type fibromatosis. Br J Surg. 2013;100(9):1214-1219. doi:10.1002/bjs.9194
- Gondim Teixeira PA, Chanson A, Verhaeghe JL, et al. Correlation between tumor growth and hormonal therapy with MR signal characteristics of desmoid-type fibromatosis: A preliminary study. Diagn Interv Imaging. 2019;100(1):47-55. doi:10.1016/j.diii.2018.06.007
- Janssen ML, van Broekhoven DL, Cates JM, et al. Meta-analysis of the influence of surgical margin and adjuvant radiotherapy on local recurrence after resection of sporadic desmoid-type fibromatosis. Br J Surg. 2017;104(4):347-357. doi:10.1002/bjs.10477
- Rampone B, Pedrazzani C, Marrelli D, Pinto E, Roviello F. Updates on abdominal desmoid tumors. World J Gastroenterol. 2007;13(45):5985-5988. doi:10.3748/wjg.v13.45.5985
- Wood TJ, Quinn KM, Farrokhyar F, Deheshi B, Corbett T, Ghert MA. Local control of extra-abdominal desmoid tumors: systematic review and meta-analysis. Rare Tumors. 2013;5(1):e2. Published 2013 Feb 11. doi:10.4081/rt.2013.e2
- Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ. WHO classification of tumours of the breast. 4th ed. Lyon: International Agency for Research on Cancer; 2012
- Abraham SC, Reynolds C, Lee JH, et al. Fibromatosis of the breast and mutations involving the APC/beta-catenin pathway [published correction appears in Hum Pathol 2002 Mar;33(3):379]. Hum Pathol. 2002;33(1):39-46. doi:10.1053/hupa.2002.30196