Abstract
Background
A 45-year-old male presented to the emergency department with right-sided abdominal pain and distention. Workup revealed a diagnosis of gallstone ileus.
Summary
A 45-year-old male with hypertension and diabetes presented to the emergency department with a two-day history of abdominal pain associated with nausea and vomiting. The physical exam was significant for abdominal distention and tenderness in the right upper and lower quadrants. Laboratory studies revealed a leukocytosis without any other abnormalities. Findings on computed tomography showed a perforated gallbladder with an air-fluid track extending to the duodenal bulb/gastric antrum. A large mass (ectopic gallstone) was located within the right lower quadrant with associated high-grade small bowel obstruction and pneumobilia (Rigler's triad). Laparotomy revealed a 4 cm gallstone in the terminal ileum for which an enterolithotomy was performed. The patient had a complete recovery after surgery and was discharged.
Conclusion
Gallstone ileus represents less than 1% of gastrointestinal obstruction cases, with higher frequency among elderly females. We present a case of gallstone ileus in a patient within a lower-prevalence population, highlighting the importance of careful assessment and management while maintaining surveillance for rare conditions.
Key Words
gallstone ileus; biliary-enteric fistula; small bowel obstruction; gallstone gastrointestinal obstruction
Case Description
Gallstone ileus is a mechanical intestinal obstruction due to gallstone impaction within the gastrointestinal tract. An initial episode of acute cholecystitis frequently precedes it; erosion and fistula formation between the gallbladder and intestinal wall is a consequence of the inflammatory process.1–3
Gallstone ileus is a rare entity that occurs in only 0.3-0.5% of patients with cholecystitis.4 In addition, it is the etiology of less than 1% of cases of intestinal obstruction.1 The patient is a 45-year-old man with hypertension and diabetes who presented to the emergency department with a two-day history of abdominal pain associated with nausea and vomiting. The patient did not have any prior surgical history.
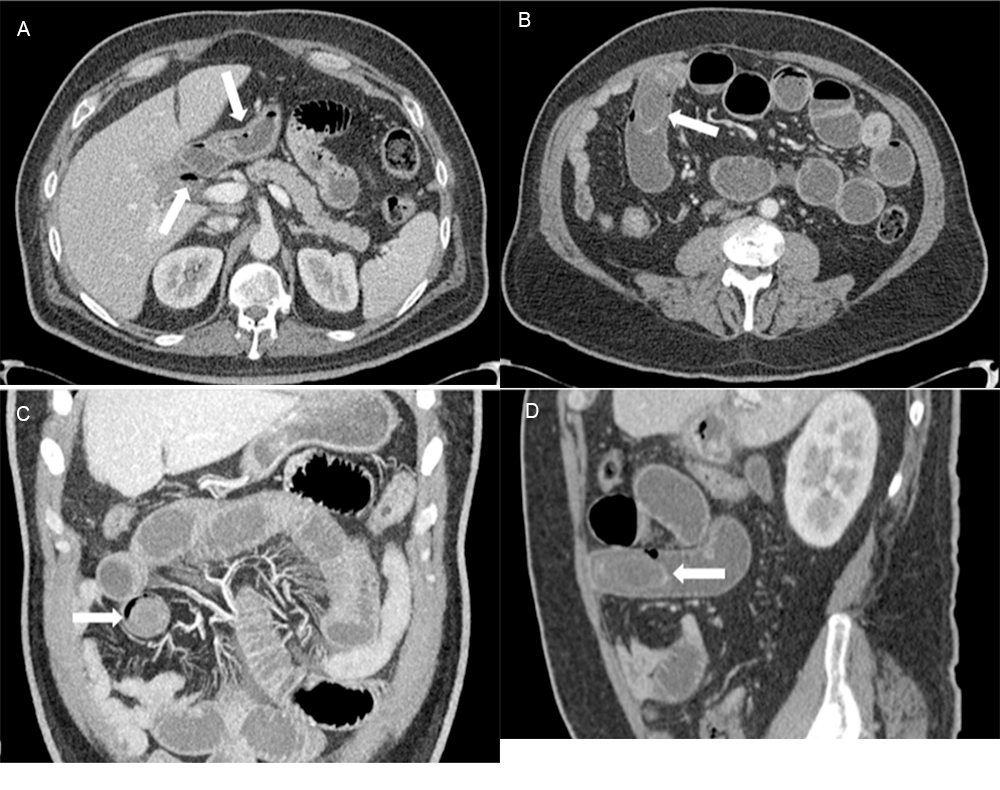
On physical examination, the patient was afebrile and in mild distress. His abdomen was distended, diffusely tender to palpation, and worse in the right upper and lower quadrants without rebound tenderness. Laboratory studies revealed a white cell count of 14,600 per microliter. The remainder of the laboratory studies were within normal limits. Computed tomography (CT) demonstrated evidence of a perforated gallbladder with an air-fluid track extending to the duodenal bulb/gastric antrum (Figure 1A). A large mass was visualized within the small bowel in the right lower quadrant, consistent with an ectopic gallstone, with associated high-grade obstruction and pneumobilia (Rigler's triad) (Figure 1B [axial], Figure 1C [coronal], and Figure 1D [sagittal]).
Figure 1. CT Scans of Perforated Gallbladder. Published With Permission
Laparotomy was performed, revealing a gallstone in the terminal ileum. A longitudinal enterotomy was made along the antimesenteric border proximal to the point of impaction. The stone was milked proximally and removed (Figure 2 and Figure 3).
Figure 2. Enterolithotomy. Published With Permission
Figure 3. Removed Gallstone. Published With Permission
The enterotomy was closed transversely in two layers. The entire length of the small bowel was examined, and no additional gallstones were found. The patient recovered well after surgery and was discharged home.
Discussion
Gallstone ileus is an uncommon cause of presentation to the emergency department. Although rare, gallstone ileus has shown a steady increase in the incidence of admissions, with higher incidence among the elderly and females.5,6 The incidence is highest in ages 60 to 84, with a female predominance ranging from 72% to 90% of patients, likely due to the increased prevalence of gallstone disease in the female gender.⁷⁻⁹ Our patient, a 45-year-old male, does not fall into either at-risk population.
Despite its infrequency, gallstone ileus possesses many facets that warrant discussion. First, the term "ileus" is a widely used misnomer because obstruction is a true mechanical phenomenon.⁶ A more appropriate term would be "gallstone gastrointestinal obstruction." Second, the cornerstone of treatment is the surgical relief of the obstruction.
The patient presented with nonspecific signs and symptoms leading to the diagnosis of small bowel obstruction, as commonly described in the literature. However, he did not present with other commonly described features of gallstone ileus, such as the intermittency of symptoms known as the "tumbling phenomenon" due to a partial obstruction followed by distal migration of the gallstone.¹
The presentation of the patient was compatible with an acute bowel obstruction, warranting a CT. CT has been demonstrated to be superior to plain abdominal films or ultrasound in diagnosing gallstone ileus.¹⁵ Findings on the first look from CT imaging included intussusception as a possible differential due to similarities in the imaging characteristics (Figure 3). The final radiologist report declared a perforated gallbladder with an air-fluid track extending to the duodenal bulb/gastric antrum. The diagnosis of gallstone ileus was most compatible with the patient's diagnostic imaging, as most fistulas occur between the gallbladder and the duodenum due to their proximity.⁹⁻¹¹
On CT imaging, the approximate size of the gallstone was 4.2 × 2.5 cm. It was located within the lumen of the small bowel in the right lower quadrant with associated proximal bowel dilation and pneumobilia. This was consistent with the characteristic Rigler's triad (1. pneumobilia; 2. small bowel obstruction; 3. ectopic gallstone), a radiologic finding leading to the diagnosis of gallstone ileus.¹⁶
In such cases, the size of the gallstone, the site of the fistula formation, and the diameter of the bowel lumen will determine the site of impaction. The gallstone can lodge in almost any part of the gastrointestinal tract, from the stomach, causing Bouveret's syndrome to the colon. If the gallstone enters the duodenum, the most common site of intestinal obstruction will be the terminal ileum and ileocecal valve.¹ This patient's gallstone was impacted in the terminal ileum, which is consistent with the literature.
The stone was of moderate size, carrying a higher tendency of impaction. Most gallstones smaller than 2.5 cm pass spontaneously through a healthy gastrointestinal tract and uneventfully into the stool.2,3,6 Gallstones larger than 5 cm are more likely to become impacted, although the spontaneous passage of gallstones as large as 5 cm has been reported.3,6,11
Once faced with gallstone ileus, there are many options for surgical management. The current surgical procedures include a simple enterolithotomy (the procedure performed in this case), a single-stage procedure, and a two-stage procedure. The one-stage procedure consists of an enterolithotomy, cholecystectomy, and fistula closure. The enterolithotomy is performed first in the two-stage procedure, followed by cholecystectomy and fistula closure in a second operation.
The most optimal procedure is heavily debated, but many authors have shown that enterolithotomy alone has better outcomes. The one-stage procedure should be reserved for select patients presenting with acute cholecystitis, gallbladder gangrene, or residual gallstone at the time of presentation and who have been clinically optimized from a cardiovascular and metabolic standpoint.9,10,17-19 In the particular scenario presented in this case, the one-stage procedure is the recommended approach due to its feasibility in a young, healthy, and hemodynamically stable patient.
Conclusion
Gallstone ileus represents less than 1% of gastrointestinal obstruction cases, with higher frequency among elderly females. We present a case of gallstone ileus in a patient within a lower prevalence population, highlighting the importance of careful assessment and management while maintaining surveillance for rare conditions.
Lessons Learned
This patient did not have the common risk factors for patients with gallstone ileus, namely elderly and female. Rare cases such as these instill the importance of a wide differential diagnosis after a well-performed physical and radiological evaluation. This case highlights the diagnostic importance of Rigler's triad and discusses the procedure of choice once the diagnosis of gallstone ileus has been made.
Authors
Jacobucci RP; Lee E; Price D; Nguyen J; Marttos A Jr; Namias N
Author Affiliation
Ryder Trauma Center, University of Miami Miller School of Medicine, Miami, FL 33136
Corresponding Author
Rodrigo P. Jacobucci, MD
Department of Surgery
Houston Methodist Hospital
6550 Fannin Street
Houston, TX 77030
Phone: (713) 441-5155
Email: rporciunculajacobucci@houstonmethodist.org
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Received: September 1, 2020
Revision received: October 21, 2020
Accepted: December 9, 2020
References
- Nuño-Guzmán CM, Marín-Contreras ME, Figueroa-Sánchez M, Corona JL. Gallstone ileus, clinical presentation, diagnostic and treatment approach. World J Gastrointest Surg. 2016;8(1):65-76. doi:10.4240/wjgs.v8.i1.65
- Fox PF. Planning the operation for cholecystoenteric fistula with gallstone ileus. Surg Clin North Am. 1970;50(1):93-102. doi:10.1016/s0039-6109(16)39035-1
- VanLandingham SB, Broders CW. Gallstone ileus. Surg Clin North Am. 1982;62(2):241-247. doi:10.1016/s0039-6109(16)42683-6
- Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77(7):737-742. doi:10.1002/bjs.1800770707
- Kurtz RJ, Heimann TM, Beck AR, Kurtz AB. Patterns of treatment of gallstone ileus over a 45-year period. Am J Gastroenterol. 1985;80(2):95-98.
- Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002;97(2):249-254. doi:10.1111/j.1572-0241.2002.05451.x
- Halabi WJ, Kang CY, Ketana N, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014;259(2):329-335. doi:10.1097/SLA.0b013e31827eefed
- Martin F. Intestinal obstruction due to gall-stones: with report of three successful cases. Ann Surg. 1912;55(5):725-743. doi:10.1097/00000658-191205000-00005
- Nakao A, Okamoto Y, Sunami M, Fujita T, Tsuji T. The oldest patient with gallstone ileus: report of a case and review of 176 cases in Japan. Kurume Med J. 2008;55(1-2):29-33. doi:10.2739/kurumemedj.55.29
- Ayantunde AA, Agrawal A. Gallstone ileus: diagnosis and management. World J Surg. 2007;31(6):1292-1297. doi:10.1007/s00268-007-9011-9
- Masannat Y, Masannat Y, Shatnawei A. Gallstone ileus: a review. Mt Sinai J Med. 2006;73(8):1132-1134.
- Warshaw AL, Bartlett MK. Choice of operation for gallstone intestinal obstruction. Ann Surg. 1966;164(6):1051-1055. doi:10.1097/00000658-196612000-00015
- Courvousier LG. Casuistisch-statistische Beitrage zue Pathologic und Chirurgie der gallenwege. XII Leipizig, FCW Vogel, 1890.
- Bouverete L. Stenose du pylore adherent a la vesicule calculeuse. Rev Med (Paris) 1896; 16: 1-16
- Yu CY, Lin CC, Shyu RY, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol. 2005;11(14):2142-2147. doi:10.3748/wjg.v11.i14.2142
- Riglers LG, Borman CN, Noble JF. Gallstone obstruction: pathogenesis and roentgen manifestations. JAMA 1941; 117:1753-1759
- Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60(6):441-446.
- Martínez Ramos D, Daroca José JM, Escrig Sos J, Paiva Coronel G, Alcalde Sánchez M, Salvador Sanchís JL. Gallstone ileus: management options and results on a series of 40 patients. Rev Esp Enferm Dig. 2009;101(2):117-124. doi:10.4321/s1130-01082009000200005
- Ravikumar R, Williams JG. The operative management of gallstone ileus. Ann R Coll Surg Engl. 2010;92(4):279-281. doi:10.1308/003588410X12664192076377