Discussion
Retrorectal abscess associated with meningocele is very rare.1–3 Meningocele is a cystic meningeal protrusion through the presacral space. Anterior meningocele can be related to some agenesis of the anterior sacrum. When associated with congenital caudal anomalies, anal stenosis and sacral defect can be part of the Currarino syndrome.4–6 Epidermoid and dermoid cysts represent 50 percent of retrorectal mass and result from defective closure of ectodermal tube; 30 percent of these cysts can become infected form an abscess with or without fistula, and are benign.
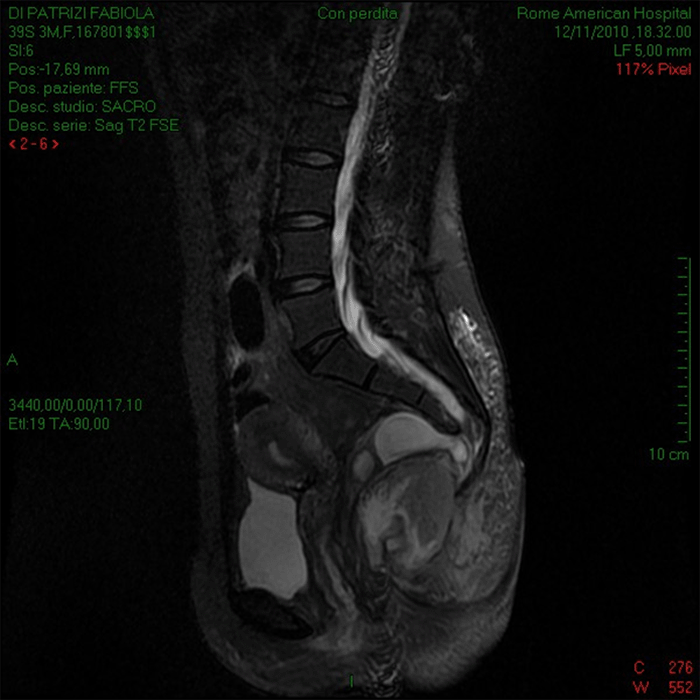
Complications of a meningocele are headache, infection with or without fistulization, rectothecal fistula, and meningitis. The symptoms of retrorectal tumors depend on the size of the mass and location. Sacral pain is a common symptom associated with fever in case of an abscess or urinary infection.7 The significance of retrorectal abscess associated with pain, fever, and severe persistent headache is presented in this unusual case presentation of retrorectal abscess and a pelvic meningocele. Pappalardo and coauthors propose a preoperative CT and an MRI anatomical and topographical classification to allow an adequate surgical approach.8
Our surgical strategy included preoperative colonoscopy to exclude possible colonic or anal origin for the abscess. This measure allowed us to approach the retrorectal abscess through a posterior incision in the coccygeal area, avoiding meningocele injury. The meningocele was asymptomatic for three years; therefore, no further surgical treatment was deemed necessary by our neurosurgeons. The histology of the abscess wall revealed an inflamed necrotic tissue; there was no confirmation of a suspected cystic origin infection. For this reason, the patient was followed up with an MRI for three years with negative radiological findings.
Conclusion
A patient with a rectal abscess mass on rectal examination associated with fever and persistent headache should undergo an MRI before surgery. This approach will help the surgeon evaluate the extent and source of the abscess and exclude the presence of a meningocele to plan a proper surgical approach and avoid possible meningitis and meningo-perineal fistula from the surgery.
Lessons Learned
When a rectal abscess mass is found on rectal examination associated with fever and persistent headache, sacral meningocele is a possibility. MRI will confirm the presence of a meningocele, assisting the surgeon in planning a procedure to avoid possible meningitis and meningo-perineal fistula.
References
- Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors. Mayo Clinic experience, 1960-1979. Dis Colon Rectum. 1985;28(9):644-652. doi:10.1007/BF02553440
- Jackman RJ, Clark PL, Smith ND. Retrorectal tumors. JAMA. 1951;145(13):956–962. doi:10.1001/jama.1951.02920310012003
- Buyukbese Sarsu S, Parmaksiz ME, Cabalar E, Karapur A, Kaya C. A very rare cause of anal atresia: Currarino syndrome. J Clin Med Res. 2016;8(5):420-423. doi:10.14740/jocmr2505w
- Lynch SA, Wang Y, Strachan T, Burn J, Lindsay S. Autosomal dominant sacral agenesis: Currarino syndrome. J Med Genet. 2000;37(8):561-566. doi:10.1136/jmg.37.8.561
- Dahan H, Arrivé L, Wendum D, Docou le Pointe H, Djouhri H, Tubiana JM. Retrorectal developmental cysts in adults: clinical and radiologic-histopathologic review, differential diagnosis, and treatment. Radiographics. 2001;21(3):575-584. doi:10.1148/radiographics.21.3.g01ma13575
- Uhlig BE, Johnson RL. Presacral tumors and cysts in adults. Dis Colon Rectum. 1975;18(7):581-589. doi:10.1007/BF02587141
- Pappalardo G, Frattaroli FM, Casciani E, et al. Retrorectal tumors: the choice of surgical approach based on a new classification. Am Surg. 2009;75(3):240-248.
Authors
Antonellis Fa; Falasco Ga; Trentino Pb; Ravo Bc
Author Affiliations
- Department of Surgery, Rome American Hospital, Rome, Italy
- San Camillo Forlanini Hospital, Università La Sapienza, Rome, Italy
- San Camillo Forlanini Hospital, Università Campus Biomedico, Rome, Italy
Corresponding Author
Biagio Ravo, MD, FACS
San Camillo Forlanini Hospital, Università Campus Biomedico
Via Emilio Longoni, 81, 00155
Rome, Italy
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no relevant financial relationships or in-kind support to disclose.
Meeting Presentation
ACS Italian Chapter Congress, Convention Center La Nuvola 14‒18, Rome, Italy, October 2018
Received: November 9, 2020
Revision received: May 17, 2021
Accepted: October 21, 2021