Discussion
Primary spontaneous pneumothorax (PSP) is a significant health problem in the United States, with an annual incidence of 18‒28 per 100,000 in males and 1.2‒6.0 per 100,000 in females.1,9 PSP most often occurs in young, tall, lean males without any underlying lung diseases primarily resulting from a ruptured subpleural bleb or bullae.1 Cigarette smoking has been identified as a major risk factor for PSP and recurrence due to its pathologic effect on the smaller airways, contributing to local emphysema and the development of bullae.1 Little is known about whether e-cigarette smoking is a safer alternative than tobacco smoking contributing to PSP; however, there has been research analyzing the toxicity of e-cigarette smoking at the cellular and biochemical level.3‒5
E-cigarettes have been growing in popularity among young adults, especially college students, with a prevalence of 1.5 percent in 2009 rising to 14 percent in 2014. Surprisingly, there was also an increase in the use of e-cigarettes in high school and middle school students from 2017 to 2018 of about 11.7 to 20.8 percent and 3.3 to 4.9 percent, respectively. According to the Food and Drug Administration (FDA), the sales of electronic nicotine delivery systems (ENDS) are only legally sold to persons of age 18 and older.10 This means that these products are easily accessible to adolescences, and the FDA's limited regulations on these substances are not well enforced.
The perception of e-cigarettes among this population revolves around their commercially touted less harmful and carcinogenic effects compared to regular tobacco smoke. Still, recent trends in manufacturing include the use of other substances in e-cigarettes other than nicotine.2 Low molecular weight aldehydes, such as acrolein, acetaldehyde, and formaldehyde, are the most toxic component in tobacco products. These have been identified in e-cigarette aerosols, raising concern over the health risk of active and passive exposure.3 Increased emission of aldehyde compounds is noted in the newer generation of e-cigarettes compared to prior generations, which directly correlates to an increase in battery power and consequently the maximum heating coil temperature of the device.3,4 Another study suggested that heating sugar constituents in e-cigarettes at different temperatures could result in different aldehyde emission profiles.4 More concerningly, most of their product labels did not list sugars or warnings about the aldehyde manufacturers are required to quantify these constituents on their labels as the FDA regulation mandates.4
Environmental exposures appear to have played a significant role in this patient's presentation given his history of mild childhood asthma and former cigarette but current marijuana and vape use. E-cigarettes cause direct damage to the lung parenchyma from the e-cigarette vapor condensate (ECVC).5 In an in vitro experiment, alveolar macrophages (AM) were exposed to either unvaped e-cigarette liquid (ECL) or ECVC. Scott et al.5 showed that ECVC resulted in more significant toxicity than ECL due to an increase in an AM inflammatory response resulting in increased apoptosis and necrosis from excessive production of reactive oxygen species (ROS) and inflammatory cytokines.5 In addition, lipid peroxidation of the cell membrane caused by the ROS can generate acrolein endogenously, further causing DNA damage of the lung parenchyma.6 In a cytological analysis by Tang et al.,6 acrolein was found to readily cross the membrane barrier and be preferentially trapped in the nucleus. This led to a reaction with DNA that inhibits its repair, resulting in either cell death or mutagenesis of the p53 tumor-suppressor gene.6 The same study found that the distribution of the Acr-DNA adduct in the p53 gene coincides with the p53 mutation pattern in cigarette smoke-related lung cancer.
As previously discussed, PSP is more common in the younger population without any underlying chronic lung diseases, which could raise the possibility of an underlying genetic etiology. The FLCN gene has at least eight mutations found to cause PSP.7 These mutations result in an abnormal folliculin protein that triggers inflammation within the lung tissue resulting in blebs.8 However, this patient's bullous disease was mainly localized to the right upper lobe. Pneumothoraces due to a genetic etiology often manifest with diffuse and bilateral bullous disease, making a genetic etiology less likely in this case.7
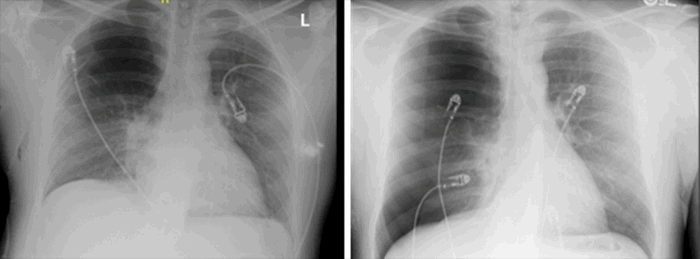
Lastly, the focus of the pulmonary blebs, in this case, is noteworthy, involving a significant portion of only the right upper lobe. It has also been proposed that one of the risk factors for spontaneous pneumothoraces in the adolescent growth spurt causes rapid growth of the chest. The peak growth occurs in the patient's mid-twenties leading to suggested vertical stress during this period, which can disrupt alveoli and cause bleb development.12,13 This has often been used to explain the apical predominance of blebs. The unilaterality of the blebs could be potentially rationalized based on pulmonary anatomy. It is well known that the location of lung infiltration after aspiration is dependent on patient positioning.11 Right upper lobe consolidation is well described in alcoholics who aspirate in the supine position.12 However, with most vaping occurring in the upright position, one might expect the right middle and lower lobes to be most affected.11 Theoretically, given that the right upper lobe bronchus is the shortest distance to the carina compared to the right intermediate bronchus and left upper lobe bronchus, inhaling the heated vapor from an e-cigarette may lead to condensation concentration of these substances in the right upper lobe.
Our patient had many risk factors for developing blebs, which subsequently led to his presentation with a pneumothorax after taking a big hit from his vape. Suppose there was indeed a genetic component that played a role. In that case, his environmental exposures could have had a synergistic effect and sped up the degenerative process within his lung parenchyma caused by aldehydes and other substances inhaled when smoking e-cigarettes.
Conclusion
Smoking is a well-known risk factor for primary spontaneous pneumothorax, for which smoking cessation is always advised. Vaping has not yet been proven to be a safer alternative to traditional smoking; however, patients should be counseled similarly and cessation encouraged. Both tobacco and e-cigarette smoking lead to the inhalation of high levels of aldehyde, which may contribute to the incidence of spontaneous pneumothorax in the young population. This case is unique due to the extent and unilaterality of the blebs seen in the right upper lobe of this patient. Spontaneous pneumothorax secondary to vaping may become more common as the prevalence of e-cigarette use increases.
Lessons Learned
Patients using e-cigarettes should be informed about the levels of aldehyde content in e-cigarette liquid products due to its absence from most product labels. They should be counseled in smoking cessation as continuation increases the risk of pulmonary comorbidities, including pneumothoraces.
Authors
Hung Fong SSab; Prince JMab; Misra Sab; Siegman Mab
Author Affiliation
- HCA/USF Morsani College of Medicine GME - Brandon, FL 33511
- HCA Florida Brandon Hospital, Brandon, FL 33511
Corresponding Author
Suy sen Hung Fong, MD
Brandon Regional Hospital
Graduate Medical Education–General Surgery
119 Oakfield Drive
Brandon, FL 33511
Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding/Support
The authors have no financial relationships or in-kind support to disclose.
Received: May 17, 2019
Revision Received: February 21, 2021
Accepted for Publication: March 4, 2021
References
- Cheng YL, Huang TW, Lin CK, et al. The impact of smoking in primary spontaneous pneumothorax. J Thorac Cardiovasc Surg. 2009;138(1):192-195. doi:10.1016/j.jtcvs.2008.12.019
- Kenne DR, Fischbein RL, Tan AS, Banks M. The use of substances other than nicotine in electronic cigarettes among college students. Subst Abuse. 2017;11:1178221817733736. Published 2017 Sep 25. doi:10.1177/1178221817733736
- Ogunwale MA, Li M, Ramakrishnam Raju MV, et al. Aldehyde detection in electronic cigarette aerosols. ACS Omega. 2017;2(3):1207-1214. doi:10.1021/acsomega.6b00489
- Fagan P, Pokhrel P, Herzog TA, et al. Sugar and aldehyde content in flavored electronic cigarette liquids. Nicotine Tob Res. 2018;20(8):985-992. doi:10.1093/ntr/ntx234
- Scott A, Lugg ST, Aldridge K, et al. Pro-inflammatory effects of e-cigarette vapour condensate on human alveolar macrophages. Thorax. 2018;73(12):1161-1169. doi:10.1136/thoraxjnl-2018-211663
- Tang MS, Wang HT, Hu Y, et al. Acrolein induced DNA damage, mutagenicity and effect on DNA repair. Mol Nutr Food Res. 2011;55(9):1291-1300. doi:10.1002/mnfr.201100148
- FLCN gene: Medlineplus genetics. MedlinePlus. https://medlineplus.gov/genetics/gene/flcn/.
- Graham RB, Nolasco M, Peterlin B, Garcia CK. Nonsense mutations in folliculin presenting as isolated familial spontaneous pneumothorax in adults. Am J Respir Crit Care Med. 2005;172(1):39-44. doi:10.1164/rccm.200501-143OC
- Lo T. Vaping And pneumothorax: a life-threatening association. Am. J. Respir. Crit. 2017;195:A2052
- Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students - United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276-1277. Published 2018 Nov 16. doi:10.15585/mmwr.mm6745a5
- Marom EM, McAdams HP, Erasmus JJ, Goodman PC. The many faces of pulmonary aspiration. AJR Am J Roentgenol. 1999;172(1):121-128. doi:10.2214/ajr.172.1.9888751
- Peters RM, Peters BA, Benirschke SK, Friedman PJ. Chest dimensions in young adults with spontaneous pneumothorax. Ann Thorac Surg. 1978;25(3):193-196. doi:10.1016/s0003-4975(10)63520-5
- Upadhyay GP, Thakker RM. Spontaneous pneumothorax – a clinical study of 100 cases. Int J Med Sci Public Health. 2017;6:154-158