At last clinical follow up, 209 days postoperatively, lipase levels had decreased to 475 U/L. There was no further evidence of panniculitis. There are no plans to treat with additional liver-directed therapy given evidence of metastasis, and the patient is managed by oncology for continued chemotherapy.
Discussion
Acinar cell carcinoma is an extremely aggressive cancer, with approximately half of patients harboring evidence of metastatic disease at the time of diagnosis.6 These neoplasms affect primarily adults with a mean age of 58 and show a striking predilection for men (male-to-female ratio 3.6:1).1 There have been seven reported cases of primary acinar cell carcinoma of the liver in the literature to date.7 Only one other reported case of primary hepatic acinar cell carcinoma associated with pancreatic panniculitis exists.7
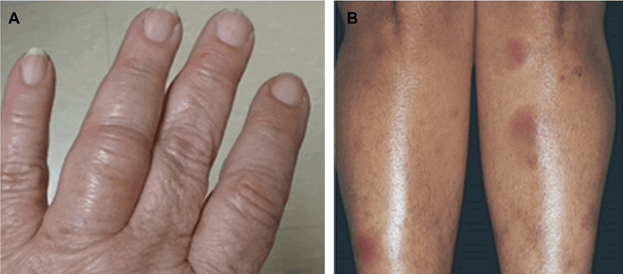
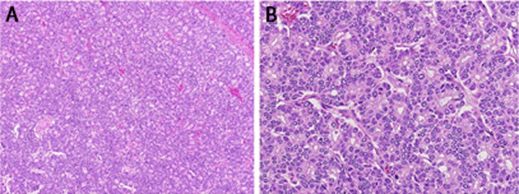
Pancreatic panniculitis has largely been associated with pancreatic diseases, including pancreatitis, pancreatic carcinomas, or intraductal papillary mucinous neoplasm (IPMN).8 Nearly 45 percent of patients with pancreatic panniculitis show subcutaneous nodules before the underlying causal disease is recognized, indicating its utility as a valuable early sign of underlying malignancies and the need to conduct further laboratory and imaging studies.9 Although the pathophysiology remains uncertain, a biopsy of panniculitis will classically demonstrate “ghost cells,” or anucleate necrotic adipocytes with a basophilic granular material within their cytoplasm, as well as inflammation.10
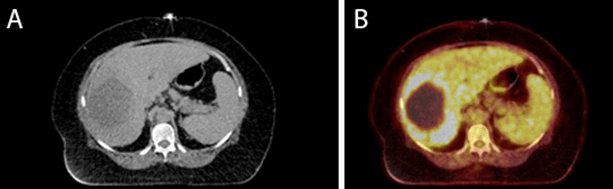
In other reported cases of extrapancreatic acinar cell carcinoma, the disease is thought to originate from metaplastic, ectopic, or transdifferentiated pancreatic tissue, sharing biologic features with primary pancreatic acinar cell carcinoma.3 In fact, acinar cells have also been found to be able to transdifferentiate into hepatocytes.11 Furthermore, both hepatocellular carcinoma and acinar cell carcinoma are often driven by a dysfunctional Wnt/β-catenin pathway. Both demonstrate a surprisingly low frequency of KRAS mutations, and the most frequent chromosomal amplifications in both tumors are found on 1q, 8q, and 20q.12 Similar to previous reports of primary hepatic acinar cell carcinoma, the tumor, in this case, lacked biliary markers and hepatocellular differentiation, displayed positivity for trypsin and BCL10, demonstrated the presence of acini with apical cytoplasmic periodic acid-Schiff (PAS)-positivity, distinct acinar structures in non-desmoplastic stroma, absence of bile, and less high-grade nuclear features, distinguishing it from other primary liver tumors.
We describe the unique case of a patient with a primary liver tumor that showed features identical to that of pancreatic acinar cell carcinoma. Her case was complicated by pancreatic panniculitis, an extremely rare occurrence in the absence of primary pancreatic disease, which resolved with resection of her tumor. Our study adds to the previous literature in demonstrating that acinar cell carcinoma of the pancreatic type may also originate from the liver and can be readily distinguished from other primary liver neoplasms through histological and immunohistochemical features. It may cause a classic presentation of pancreatic panniculitis, an indicator of extremely high lipase levels, and possible presenting symptom of underlying malignancy, especially acinar cell carcinoma, of which practicing clinicians should be wary.
Conclusion
Pancreatic panniculitis is a rare complication of a rare cancer, namely acinar cell carcinoma. We present a unique case of extrapancreatic acinar cell carcinoma complicated by pancreatic panniculitis, which resolved with surgical resection of the underlying disease. It highlights the importance of considering extrapancreatic disease in the differential diagnosis of pancreatic panniculitis.
Lessons Learned
The presence of painful subcutaneous nodules that do not resolve with standard topical therapy should prompt consideration of the diagnosis of pancreatic panniculitis. This diagnosis is crucial, as it may further signify the presence of an extremely aggressive underlying malignancy, acinar cell carcinoma.
Authors
Jairath NKa; Jairath Ra; Westerhoff Mb; Nathan Ha
Author Affiliations
- University of Michigan, Department of Surgery, Ann Arbor, MI 48109
- University of Michigan, Department of Pathology, Ann Arbor, MI 48109
Corresponding Author
Neil Kunal Jairath
University of Michigan, Department of Surgery
Cancer Center, Floor B1, Reception E
1500 E Medical Center Drive SPC 5912
Ann Arbor, MI 48109
Phone: (734) 647-8902
E-mail: jairathn@med.umich.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
Acknowledgements
This manuscript was supported by unrestricted departmental support from the department of surgery and surgical oncology at the University of Michigan.
References
- Hruban R, Pitman M, Klimstra D. Tumors of the Pancreas. 4th Series, Fascicle 6. Washington; American Registry of Pathology, American Registry of Pathology and Armed Forces Institute of Pathology, Washington, DC; 2007. AFIP Atlas of Tumor Pathology.
- Agaimy A, Kaiser A, Becker K, et al. Pancreatic-type acinar cell carcinoma of the liver: a clinicopathologic study of four patients. Mod Pathol. 2011;24(12):1620-1626. doi:10.1038/modpathol.2011.127
- Lee H, Tang LH, Veras EF, Klimstra DS. The prevalence of pancreatic acinar differentiation in gastric adenocarcinoma: report of a case and immunohistochemical study of 111 additional cases. Am J Surg Pathol. 2012;36(3):402-408. doi:10.1097/PAS.0b013e318238369e
- Sun Y, Wasserman PG. Acinar cell carcinoma arising in the stomach: a case report with literature review. Hum Pathol. 2004;35(2):263-265. doi:10.1016/j.humpath.2003.09.020
- Makhlouf HR, Almeida JL, Sobin LH. Carcinoma in jejunal pancreatic heterotopia. Arch Pathol Lab Med. 1999;123(8):707-711. doi:10.5858/1999-123-0707-CIJPH
- Kitagami H, Kondo S, Hirano S, Kawakami H, Egawa S, Tanaka M. Acinar cell carcinoma of the pancreas: clinical analysis of 115 patients from Pancreatic Cancer Registry of Japan Pancreas Society. Pancreas. 2007;35(1):42-46. doi:10.1097/mpa.0b013e31804bfbd3
- Zundler S, Erber R, Agaimy A, et al. Pancreatic panniculitis in a patient with pancreatic-type acinar cell carcinoma of the liver--case report and review of literature. BMC Cancer. 2016;16:130. Published 2016 Feb 20. doi:10.1186/s12885-016-2184-6
- Marsh Rde W, Hagler KT, Carag HR, Flowers FP. Pancreatic panniculitis. Eur J Surg Oncol. 2005;31(10):1213-1215. doi:10.1016/j.ejso.2005.06.007
- Dahl PR, Su WP, Cullimore KC, Dicken CH. Pancreatic panniculitis. J Am Acad Dermatol. 1995;33(3):413-417. doi:10.1016/0190-9622(95)91385-8
- Laureano A, Mestre T, Ricardo L, Rodrigues AM, Cardoso J. Pancreatic panniculitis - a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. 2014;8(1):35-37. Published 2014 Mar 31. doi:10.3315/jdcr.2014.1167
- Shen CN, Tosh D. Transdifferentiation of pancreatic cells to hepatocytes. Methods Mol Biol. 2010;640:273-280. doi:10.1007/978-1-60761-688-7_14
- Ghurburrun E, Borbath I, Lemaigre FP, Jacquemin P. Liver and pancreas: do similar embryonic development and tissue organization lead to similar mechanisms of tumorigenesis?. Gene Expr. 2018;18(3):149-155. doi:10.3727/105221618X15216414278706