Discussion
Traumatic extrapleural hematomas were first described by Lipchik and Robinson in 19681 and further defined by Rashid et al. in 2000 in a case series of 34 patients.1 Here we present a case of a patient without any history of blood thinning medications who suffered blunt chest wall trauma, was initially asymptomatic, and then developed a late onset EPH leading to tension physiology necessitating emergent operative exploration and hematoma evacuation using a VATS approach. To our knowledge, this is the first report of tension physiology secondary to a delayed EPH.
Minimally invasive treatment options for EPHs include transcatheter arterial embolization (TAE) and VATS. TAE has been shown in multiple case reports to be a viable treatment modality for stable patients with EPH and has the benefit of avoiding the risks of a more extensive operation.5-7 In unstable patients and patients with an expanding EPH at risk for tension physiology, TAE is insufficient as it does not remove the hematoma nor relieve the pressure on the mediastinal structures.
The operative technique in prior case reports utilizing VATS for EPH involves entering the pleural cavity and then draining the hematoma intrapleurally with a partial pleurectomy if a connection was not already present.3,7,8 In contrast to this, the present case was managed with initial direct drainage of the extrapleural hematoma without entering the thoracic cavity, permitting immediate decompression of the hematoma, thereby stabilizing the patient. The pleural space could then be entered in a safe and controlled fashion. Further exploration then ensured there was no hemothorax component and allowed the remaining hematoma to be drained intrapleurally with a partial pleurectomy. In patients with tension physiology, this approach may decrease the time required to reduce the intrathoracic pressure and correct the underlying pathophysiology.
Conclusion
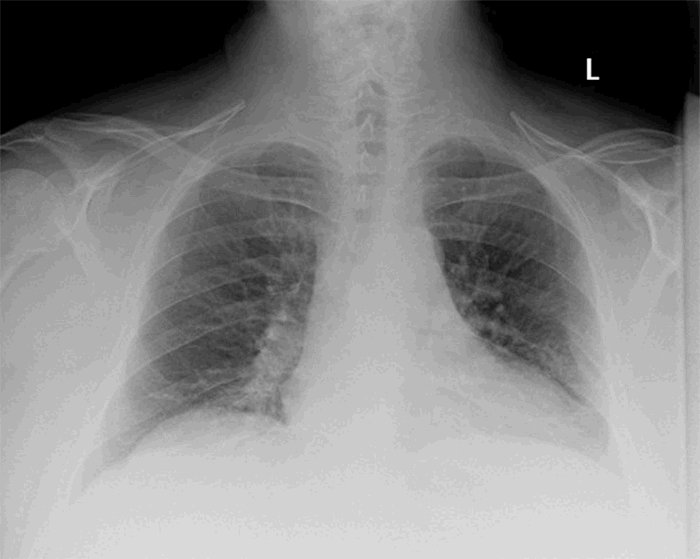
Delayed presentation of EPHs is a relatively rare complication of thoracic trauma in which an initially asymptomatic patient can present with life-threatening tension physiology several days after their injury. All patients, even asymptomatic, with rib fractures or at risk for missed rib fractures on initial imaging should have routine follow-up chest radiograph for monitoring their injuries as well as for rare complications such as EPHs. Minimally invasive techniques are effective for these patients, and unstable patients or those with tension physiology should be taken for VATS. Consideration should be given to initial extrapleural drainage before entering the thoracic cavity to more quickly relieve intrathoracic pressure and alleviate tension physiology if present.
Lessons Learned
Late-onset extrapleural hematomas may present with tension physiology following blunt chest trauma. Immediate operation is prudent and can be safely done with minimally invasive techniques.
Authors
Murray CR; Simon BJ; DeBusk MG
Author Affiliation
University of Massachusetts Medical School
Department of Surgery
Worcester, MA 01655
Corresponding Author
M. George DeBusk, MD, MSc, FACS
UMass Memorial Medical Center, S3-711
Department of Surgery
55 Lake Avenue North
Worcester, MA 01655
Phone: (508) 856-1168
E-mail: george.debusk@umassmemorial.org
Disclosure Statement
The authors have no conflicts of interest to disclose.
Acknowledgements
We would like to thank Karl Uy, MD, FACS, for providing technical and writing assistance.
References
- Lipchik, E O, and K E Robinson. “Acute traumatic rupture of the thoracic aorta.” The American journal of roentgenology, radium therapy, and nuclear medicine vol. 104,2 (1968): 408-12. doi:10.2214/ajr.104.2.408
- Rashid, M A et al. “Nomenclature, classification, and signficance of traumatic extrapleural hematoma.” The Journal of trauma vol. 49,2 (2000): 286-90. doi:10.1097/00005373-200008000-00016
- Masuda, Ryota et al. “Delayed hemothorax superimposed on extrapleural hematoma after blunt chest injury: a case report.” The Tokai journal of experimental and clinical medicine vol. 38,3 97-102. 20 Sep. 2013
- Pirzirenli, Mehmet Gökhan et al. “Extrapleural hematoma cases treated with video-assisted thoracoscopic surgery.” Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery : TJTES vol. 21,5 (2015): 405-9. doi:10.5505/tjtes.2015.38768
- Morita, S et al. “Atypical extravasation of contrast medium in massive extrapleural haematoma due to cardiac massage without rib fracture.” Emergency medicine journal : EMJ vol. 26,10 (2009): 710. doi:10.1136/emj.2008.061739
- Gorospe, Luis et al. “Nonoperative Management of a Large Extrapleural Hematoma after Blunt Chest Trauma.” The Journal of emergency medicine vol. 51,2 (2016): 159-63. doi:10.1016/j.jemermed.2016.02.027
- Morita, Seiji et al. “Arterial embolization of an extrapleural hematoma from a dislocated fracture of the lumbar spine: a case report.” Scandinavian journal of trauma, resuscitation and emergency medicine vol. 17 27. 9 Jun. 2009, doi:10.1186/1757-7241-17-27
- Igai, Hitoshi et al. “Rapidly expanding extrapleural hematoma.” General thoracic and cardiovascular surgery vol. 56,10 (2008): 515-7. doi:10.1007/s11748-008-0284-1