Discussion
The incidence of PVT after laparoscopic sleeve gastrectomy has been reported to be between 0.3 and 1 percent.1,2 PVT occurs more commonly after LSG than any other bariatric procedure.1–4 There are only a few reported cases of PMVT following bariatric surgery in the existing literature5–13; the first LSG-related PMVT was reported by Berthet et al. in 2009.14 The majority of patients who do develop PVT following bariatric surgery have a positive thrombophilia study with evidence of some genetic coagulopathy.15–17 However, morbid obesity in and of itself is a predisposing factor for post-operative venous thrombosis. According to the Modified Caprini Risk Assessment tool for assessment of VTE risk, virtually all bariatric patients are at moderate risk (three percent risk without mechanical or chemical prophylaxis) for VTE.18 To mitigate this risk, the journal Surgery for Obesity and Related Diseases recommend unfractionated heparin or low-molecular weight heparin preoperatively plus the use of sequential compression devices during the recovery period.19 The patient received these precautions. However, the guidelines are unclear about anticoagulation after patients are discharged from the hospital.
Multiple suggestions have been offered to explain the pathogenesis of PMVT preferentially following LSG as opposed to other laparoscopic bariatric procedures. These include (1) splenic ischemia from ligation of the short gastric vessels; (2) endothelial damage from thermal effect on the left gastroepiploic vessel during skeletonization of the greater curvature; and (3) hepato-splanchnic congestion from liver retraction for a prolonged period of time.1–3,15,20 Furthermore, the author noted that ligation of the short gastric veins as well as skeletonization of the greater curvature is expected to result in (1) a reduction in the respective pressure differentials between the splenic vein to the portal vein and gastro-epiploic vein to the portal vein in the direction of venous flow as well as (2) an increase in resistance, thereby slowing venous flow according to Ohm’s law (flow = pressure differential/total resistance). In a patient undergoing laparoscopic surgery already being exposed to endothelial damage by thermal ligation, an underlying genetic coagulopathy completes Virchow’s triad for thrombosis: flow stasis, endothelial damage, and hypercoagulability.
The treatment of PMVT in our patient required careful consideration of three management options: conservative anticoagulation therapy, catheter-directed thrombolysis, and thrombectomy.21–23 Without prompt initial anticoagulation, risks include intestinal ischemia, infarction, and ultimately necrosis and/or acute pylephlebitis.24 Asymptomatic PVT may remain undetected until it becomes chronic and causes portal hypertension evidenced by the development of venous collaterals, or “cavernous portal transformation.” Thrombectomy is generally reserved for severe cases that necessitate taking the patient back to the operating room (intestinal necrosis).
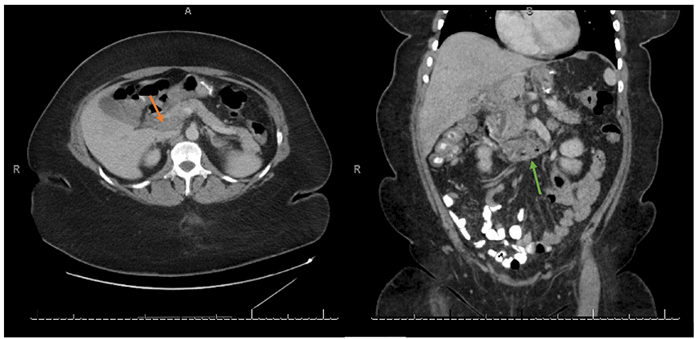
Catheter-directed thrombolysis has been emerging as a practical option to recanalization of acute PVT without intestinal infarction.22,23 Thrombolysis can be performed percutaneously through various approaches: transjugular, transhepatic, transsplenic, transileocolic, and omental vein.25–28 In the transjugular approach, the portal vein is accessed from one of the hepatic veins or the inferior vena cava. Transhepatic access carries an increased risk of bleeding in the setting of thrombolytic therapy. The transileocolic approach requires surgical access. For this patient with evidence suggestive of diffuse mesenteric venous thrombosis, indirect access through the superior mesenteric artery via the common femoral artery was the preferred approach.29
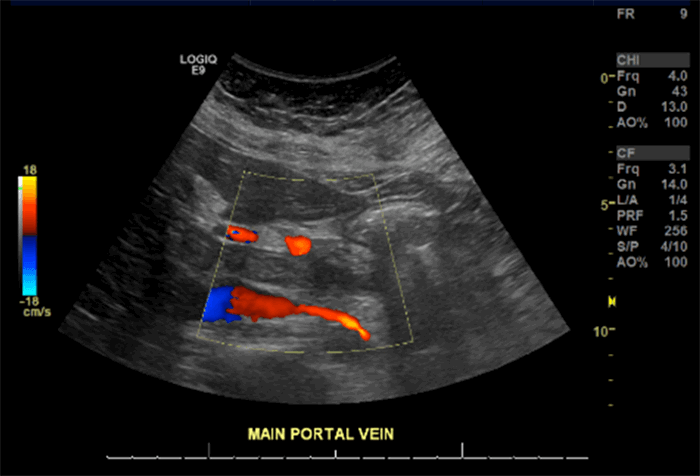
Recanalization for the patient was successfully achieved by catheter-directed lysis with tissue plasminogen activator, and similar successful lysis of acute PVT has been reported elsewhere.30,31 However, given that the patient did not develop ischemia but did develop portal cavernous transformation at six months, there is a question of whether enough recanalization was achieved. This patient will now need to be followed closely to screen for varices or other consequences of portal hypertension as well as malignant transformations. Further exploration of this management approach with controlled prospective trials are needed to determine its efficacy in comparison to therapeutic low-molecular weight heparin alone.
Furthermore, this case invokes the utility of VTE prophylaxis, defined as prophylactic anticoagulation for one to four weeks postoperatively. The patient’s clot developed well into the postoperative period, and although there seems to be a consensus on preventing perioperative thrombosis, there is minimal level I evidence to recommend a dose or duration of therapy for extended VTE prophylaxis after discharge.2,19,32 The patient had no history of previous thrombotic event, no known risk factors, and did not have a previously diagnosed coagulopathy; she was therefore not given postdischarge prophylaxis. Thrombophilia workup was only positive for a mild elevation in apolipoprotein A that has been associated with prothrombotic fibrin clot phenotype contributing to arterial disease33 but has not been proven to increase venous thrombosis risk.34,35
For this patient, the authors recommended long-term anticoagulation with follow-up imaging to avoid significantly increasing her risk for major bleeding. The rate of major bleeding with indefinite anticoagulation was estimated to be 2.7 per 100 patient-years in one meta-analysis.36 In general, it is not recommended to initiate indefinite anticoagulation in patients with a first-time provoked VTE due to a transient risk factor such as surgery. For such patients, the VTE recurrence risk without anticoagulation is estimated to be one percent at one year and three percent at five years.37–39 Current evidence suggests it is generally acceptable to anti-coagulate for three to six months and repeat imaging studies in a patient similarly at minimal risk for major bleeding and does not have indications for lifelong therapy (e.g., genetic coagulopathy, recurrent VTE, unprovoked VTE).19,21
Conclusion
Virtually all bariatric patients are at least at moderate risk for developing venous thrombosis during the perioperative period. As the symptoms of portomesenteric venous thrombosis are nonspecific, a high index of suspicion is necessary for diagnosis during the extended postoperative period. This case highlights the need for prospective controlled trials to identify those patients who might benefit from extended VTE prophylaxis, and to study the efficacy of catheter-directed thrombolysis.
Lessons Learned
Postoperative portomesenteric venous thrombosis is a rare complication associated with laparoscopic sleeve gastrectomy, more so than with other bariatric procedures. There is currently minimal evidence to recommend which patients may benefit from continuing chemical thromboprophylaxis postdischarge to prevent this condition. A high index of suspicion is necessary for diagnosis as the symptoms are nonspecific.
Authors
Buyukozturk Ba; Cohen Bb
Corresponding Author
Berna Buyukozturk
Florida Atlantic University
777 Glades Rd, Building 71
Boca Raton, FL 33431
Phone: bbuyukozturk2020@gmail.com
E-mail: (954) 850-7211
Author Affiliations
a Charles E. Schmidt College of Medicine, Florida Atlantic University, Boca Raton, FL 33431
b Memorial Regional Hospital, Division of General and Bariatric Surgery, Hollywood, FL 33021
Meeting Presentation
South Florida Chapter, American College of Surgeons 2019 Annual Meeting, Memorial Regional Hospital, Hollywood, FL, March 2019
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Shoar S, Saber AA, Rubenstein R, et al. Portomesentric and splenic vein thrombosis (PMSVT) after bariatric surgery: a systematic review of 110 patients. Surg Obes Relat Dis. 2018;14(1):47-59. doi:10.1016/j.soard.2017.09.512
- Tan SBM, Greenslade J, Martin D, Talbot M, Loi K, Hopkins G. Portomesenteric vein thrombosis in sleeve gastrectomy: a 10-year review. Surg Obes Relat Dis. 2018;14(3):271-275. doi:10.1016/j.soard.2017.12.010
- Husain FA. Comment on: portomesenteric vein thrombosis in sleeve gastrectomy: a 10 year review. Surg Obes Relat Dis. 2018;14(3):276. doi:10.1016/j.soard.2018.01.007
- Karaman K, Aziret M, Bal A, Öter V, Ercan M, Bostancı EB. Porto-mesenteric venous thrombosis after laparoscopic sleeve gastrectomy: A case report and systematic review of the 104 cases. Obes Res Clin Pract. 2018;12(3):317-325. doi:10.1016/j.orcp.2017.12.002
- Huerta S, Li Z, Livingston EH. Outcome of portal injuries following bariatric operations. Obes Surg. 2006;16(1):105-109. doi:10.1381/096089206775222203
- Denne JL, Kowalski C. Portal vein thrombosis after laparoscopic gastric bypass. Obes Surg. 2005;15(6):886-889. doi:10.1381/0960892054222650
- Johnson CM, de la Torre RA, Scott JS, Johansen T. Mesenteric venous thrombosis after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2005;1(6):580-583. doi:10.1016/j.soard.2005.08.001
- De Roover A, Detry O, Coimbra C, Hamoir E, Honoré P, Meurisse M. Pylephlebitis of the portal vein complicating intragastric migration of an adjustable gastric band. Obes Surg. 2006;16(3):369-371. doi:10.1381/096089206776116363
- Calmes JM, Bettschart V, Raffoul W, Suter M. Band infection with splenoportal venous thrombosis: an unusual but severe complication of gastric banding. Obes Surg. 2002;12(5):699-702. doi:10.1381/096089202321019729
- Swartz DE, Felix EL. Acute mesenteric venous thrombosis following laparoscopic Roux-en-Y gastric bypass. JSLS. 2004;8(2):165-169.
- Sonpal IM, Patterson L, Schreiber H, Benmeir A. Mesenteric venous thrombosis after gastric bypass. Obes Surg. 2004;14(3):419-421. doi:10.1381/096089204322917972
- Bellanger DE, Hargroder AG, Greenway FL. Mesenteric venous thrombosis after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2010;6(1):109-111. doi:10.1016/j.soard.2009.08.004Singh P, Sharma M, Gandhi K, Nelson J, Kaul A. Acute mesenteric vein thrombosis after laparoscopic gastric sleeve surgery for morbid obesity. Surg Obes Relat Dis. 2010;6(1):107-108. doi:10.1016/j.soard.2009.08.003
- Berthet B, Bollon E, Valero R, Ouaissi M, Sielezneff I, Sastre B. Portal vein thrombosis due to factor 2 leiden in the post-operative course of a laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19(10):1464-1467. doi:10.1007/s11695-009-9910-y
- Salinas J, Barros D, Salgado N, et al. Portomesenteric vein thrombosis after laparoscopic sleeve gastrectomy. Surg Endosc. 2014;28(4):1083-1089. doi:10.1007/s00464-013-3055-8
- Bain K, Kassapidis V, Meytes V, Ferzli G. Portomesenteric vein thrombosis following laparoscopic sleeve gastrectomy: are underlying haematological disorders the culprit?. BMJ Case Rep. 2018;2018:bcr2017223937. Published 2018 Feb 23. doi:10.1136/bcr-2017-223937
- Kumar S, Sarr MG, Kamath PS. Mesenteric venous thrombosis. N Engl J Med. 2001;345(23):1683-1688. doi:10.1056/NEJMra010076
- Gould MK, Garcia DA, Wren SM, et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines [published correction appears in Chest. 2012 May;141(5):1369]. Chest. 2012;141(2 Suppl):e227S-e277S. doi:10.1378/chest.11-2297
- American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis. 2013;9(4):493-497. doi:10.1016/j.soard.2013.03.006
- Villagrán R, Smith G, Rodriguez W, et al. Portomesenteric Vein Thrombosis After Laparoscopic Sleeve Gastrectomy: Incidence, Analysis and Follow-Up in 1236 Consecutive Cases. Obes Surg. 2016;26(11):2555-2561. doi:10.1007/s11695-016-2183-3
- Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32(3):466-470. doi:10.1053/jhep.2000.16597
- Hall TC, Garcea G, Metcalfe M, Bilku D, Dennison AR. Management of acute non-cirrhotic and non-malignant portal vein thrombosis: a systematic review. World J Surg. 2011;35(11):2510-2520. doi:10.1007/s00268-011-1198-0
- Hollingshead M, Burke CT, Mauro MA, Weeks SM, Dixon RG, Jaques PF. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005;16(5):651-661. doi:10.1097/01.RVI.0000156265.79960.86
- Joh JH, Kim DI. Mesenteric and portal vein thrombosis: treated with early initiation of anticoagulation. Eur J Vasc Endovasc Surg. 2005;29(2):204-208. doi:10.1016/j.ejvs.2004.10.005
- Bertram H, Pfister ED, Becker T, Schoof S. Transsplenic endovascular therapy of portal vein stenosis and subsequent complete portal vein thrombosis in a 2-year-old child. J Vasc Interv Radiol. 2010;21(11):1760-1764. doi:10.1016/j.jvir.2010.06.025
- Bilbao JI, Elorz M, Vivas I, Martínez-Cuesta A, Bastarrika G, Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovasc Intervent Radiol. 2004;27(5):474-480. doi:10.1007/s00270-004-0241-z
- Fonseca AL, Cleary MA, Cholewczynski W, et al. Omental vein catheter thrombolysis for acute porto-mesenteric vein thrombosis
- Liu FY, Wang MQ, Duan F, Wang ZJ, Song P. Interventional therapy for symptomatic-benign portal vein occlusion. Hepatogastroenterology. 2010;57(104):1367-1374.
- Chamarthy MR, Anderson ME, Pillai AK, Kalva SP. Thrombolysis and Transjugular Intrahepatic Portosystemic Shunt Creation for Acute and Subacute Portal Vein Thrombosis. Tech Vasc Interv Radiol. 2016;19(1):42-51. doi:10.1053/j.tvir.2016.01.005
- Blum U, Haag K, Rössle M, et al. Noncavernomatous portal vein thrombosis in hepatic cirrhosis: treatment with transjugular intrahepatic portosystemic shunt and local thrombolysis. Radiology. 1995;195(1):153-157. doi:10.1148/radiology.195.1.7892458
- Cherukuri R, Haskal ZJ, Naji A, Shaked A. Percutaneous thrombolysis and stent placement for the treatment of portal vein thrombosis after liver transplantation: long-term follow-up. Transplantation. 1998;65(8):1124-1126. doi:10.1097/00007890-199804270-00018
- Caruso F, Cesana G, Lomaglio L, et al. Is Portomesenteric Vein Thrombosis After Laparoscopic Sleeve Gastrectomy Related to Short-Course Prophylaxis of Thromboembolism? A Monocentric Retrospective Analysis About an Infrequent but Not Rare Complication and Review of the Literature. J Laparoendosc Adv Surg Tech A. 2017;27(10):987-996. doi:10.1089/lap.2017.0190
- Boffa MB, Koschinsky ML. Lipoprotein (a): truly a direct prothrombotic factor in cardiovascular disease?. J Lipid Res. 2016;57(5):745-757. doi:10.1194/jlr.R060582
- van Schouwenburg IM, Mahmoodi BK, Gansevoort RT, et al. Lipid levels do not influence the risk of venous thromboembolism. Results of a population-based cohort study. Thromb Haemost. 2012;108(5):923-929. doi:10.1160/TH12-06-0426
- Chamberlain AM, Folsom AR, Heckbert SR, Rosamond WD, Cushman M. High-density lipoprotein cholesterol and venous thromboembolism in the Longitudinal Investigation of Thromboembolism Etiology (LITE). Blood. 2008;112(7):2675-2680. doi:10.1182/blood-2008-05-157412
- Linkins LA, Choi PT, Douketis JD. Clinical impact of bleeding in patients taking oral anticoagulant therapy for venous thromboembolism: a meta-analysis. Ann Intern Med. 2003;139(11):893-900. doi:10.7326/0003-4819-139-11-200312020-00007
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines [published correction appears in Chest. 2012 Dec;142(6):1698-1704]. Chest. 2012;141(2 Suppl):e419S-e496S. doi:10.1378/chest.11-2301 Baglin T, Bauer K, Douketis J, et al. Duration of anticoagulant therapy after a first episode of an unprovoked pulmonary embolus or deep vein thrombosis: guidance from the SSC of the ISTH. J Thromb Haemost. 2012;10(4):698-702. doi:10.1111/j.1538-7836.2012.04662.x
- Nicolaides AN, Fareed J, Kakkar AK, et al. Prevention and treatment of venous thromboembolism--International Consensus Statement. Int Angiol. 2013;32(2):111-260.