Figure 3. Endoscopic appearance of near circumferential, fungating and friable sigmoid mass.
The sigmoid colon was dissected free from the abdominal wall, revealing the fistulous connection to the left flank. The abdominal wall excised back to healthy tissue, but due to the necrotic nature of the tissue, frozen sections were not pursued. The tumor also formed fistulae to the bladder wall and to the terminal ileum, approximately 20 cm from the ileocecal valve. Fifteen centimeters of the terminal ileum was resected with the colon specimen. The fistula to the bladder was then excised. A leak test was performed which did not show any clear defect, so no repair was necessary. A left hemicolectomy with transverse end colostomy was ultimately performed.
Pathology of the sigmoid mass revealed a 6-cm x 5-cm moderately differentiated adenocarcinoma with clear margins and 0/19 lymph nodes positive consistent with pT4bN0M0 consistent with stage IIC. Within the resected ileum, extensive serosal adhesive disease with inflammation and mural abscesses was encountered though devoid of malignant extension. Following multiple washouts and debridements, her flank wound was eventually closed. Post-operatively she recovered well. Adjuvant chemotherapy with capecitabine was initiated due to concern for residual tumor in the abdominal wall.
Discussion
Though colorectal cancer is complicated by spontaneous perforation in up to 12% of cases, fistulas are an uncommon occurrence, albeit a recognized complication.1,2,3,8,11 Fistulous complications occur in less than 10% of colon cancers as a result of locally advanced disease.1 Patients with fistulous complications typically present with gastrointestinal hemorrhage, and obstruction. In contrast, our patient presented with non-specific symptoms of flank pain and fatigue. Fistulizing colonic adenocarcinoma occur most often in the sigmoid colon and can involve adjacent colon (colocolic), urinary bladder (colovesical), small intestine (coloenteric), abdominal wall (colocutaneous) and/or vagina (colovaginal).2,5 Among patients with sigmoid colon cancer, approximately 20% develop fistulas as a result of local necrosis. Fistulas are associated with intra-abdominal abscesses approximately 44% of the time.10 The morbidity associated with fistulous disease can be minimized early as the formation of fistulae are a late complication of detection of tumor growth.6
Patients with fistulous complications may be asymptomatic but usually present with systemic illness, abdominal or urinary complaints, depending on the involved organs and patency of the fistulous tracts. Sepsis, volume depletion, electrolyte imbalances, and bleeding are the most common presenting symptoms. As an example, coloenteric fistulas can present with diarrhea and nutrient deficiencies. Diarrhea may be caused by short bowel syndrome, bile salt deficiency, or small intestinal bacterial overgrowth. Malnutrition and micronutrient deficiencies can present with macrocytic anemia, alopecia, dermatitis, night blindness, cachexia and unintentional weight loss.7,9,10 Colovaginal and colovesicular fistulas often present with feculent vaginal fluid or urine, respectfully.
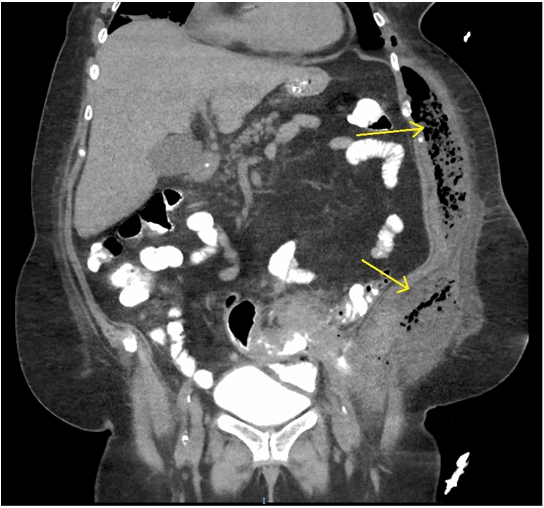
Etiologies for sigmoid fistulous disease includes colonic adenocarcinoma, complicated diverticulitis, Crohn's disease, stercoral ulcerations, vasculitis and ischemia. In addition to history and physical examination, abdominal CT and endoscopy are often sufficient for diagnosis and should be utilized early in presentation. CT is the most accurate modality in demonstrating small fistulous tracts which appear as mucosal wall thickening with adjacent inflammatory changes/pericolic fat stranding with associated air pockets. Endoscopy has advantages of direct visualization with tissue acquisition. With the addition of fluoroscopy, it is possible, although sometimes difficult to localize fistulae if not conspicuous.4 Treatment focuses on addressing the underlying etiology, as in our case with early definitive surgical infection control, tumor resection, staging, and adjuvant chemotherapy.
Rarely do patients have fistulous complications as an initial presentation of their colon cancer. We speculate that this patient's colon adenocarcinoma had an exuberant inflammatory component given extensive fistulizing disease without local or distant metastasis.
Conclusion
This case highlights that locally advanced colonic adenocarcinoma may present with fistulous complications and subtle subjective complaints. To our knowledge this is the first reported case of a patient initially presenting with multiple fistulous complications as a result of a locally advanced sigmoid adenocarcinoma.
Lessons Learned
The presence of fistulous complications associated with sigmoid adenocarcinoma does not necessarily indicate metastatic disease. Early detection of colonic neoplasm can minimize morbidities associated with surgical management to repair fistulous complications.
Authors
Zachary S. Neubert, DO
Naval Medical Center San Diego
United States Navy
Departments of Gastroenterology & Surgery
San Diego, CA
Jan-Michael Van Gent, DO
Naval Medical Center San Diego
United States Navy
Departments of Gastroenterology & Surgery
San Diego, CA
R. Daniel Lawson, MD
Naval Medical Center San Diego
United States Navy
Departments of Gastroenterology & Surgery
San Diego, CA
Correspondence Author
MAJ Zachary S. Neubert, DO
United States Navy
Department of Gastroenterology
Naval Medical Center San Diego
San Diego, CA 92134
Phone: 619-253-9725
Email: zachary.s.neubert.mil@mail.mil
Disclosure Statement
The authors have no conflicts of interest to disclose.
The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. Government.
References
- Yamada K, Miyakura Y, Koinuma K, Horie H, Lefor A, Yasuda Y, Fukushima N, Oyama Y, Nemoto Y, Azuma H. Primary and secondary adenocarcinomas associated with anal fistulae, Surgery Today. 2014;44:5.
- Lim C, Kim S, Kim J, Cho Y, Park J, Lee I. Successful palliation of a gastrocolic fistula secondary to gastric cancer by insertion of a covered colonic stent. Gastrointest Endosc. 2011;73:1314-1317.
- Nagaraja R, Kudva A, Prasad N. Spontaneous colocutaneous fistula: A rare presentation of colon carcinoma. Internet J Surg. 2008;15:1.
- Speights V, Johnson M, Stoltenberg P, Rappaport E, Helbert B, Riggs M. Colorectal cancer: Current trends in initial clinical manifestations. South Med J. 1991;84:575-578.
- Tenreiro N, Ferreira C Silva S. Locally advanced colon cancer with cutaneous invasion: case report. BMC Res Notes. 2017;10:113.
- Jethwani U, Bansal A, Kandwal V. Spontaneous enterocutaneous fistula due to colonic malignancy: A rare case report. Archives of International Surgery. 2013;3:147-149.
- Vergara-Fernandez O, Gutierrez-Grobe Y, Lavenant-Borja Y. Gastrocolic fistula secondary to adenocarcinoma of the transverse colon: a case report. J Med Case Rep. Oct 2015;27:9:263.
- Zanghi G, Leanza V, Vecchio R. Neoplastic sigmoid-uterine fistula. An exceptional complication of large intestine cancer. G Chir. Jan 2017;38:37-40.
- Zhou B, WeiHua L. A Case of Gastrocolic Fistula Secondary to adenocarcinoma of the colon. International Journal of Surgery Case Reports. 2015;15:46-49.
- Griseldan P, Rudresh H, Aishwaryab K, Tippani D, Aruna C. Malignant Colojejunal Fistula First Discovered on CT: A Case Report. J Clin Diagn Res. Nov 2014;8(11):01-03.
- Wadhwani N, Deepak K. Localised perforation of locally advanced transverse colon cancer with spontaneous colocutaneous fistula formation: a clinical challenge. BMJ Case Reports. Apr2018.