There was no other evidence of metastatic disease in the peritoneal cavity. The pathology report was consistent with moderately differentiated colonic adenocarcinoma involving the colonic wall and adjacent skin and subcutaneous tissue. All margins were tumor-free.
Discussion
Although recurrent colon and rectal cancer is common, rectal cancer with isolated recurrence at the colostomy site is rarely encountered. We generated a PUBMED and MEDLINE search for recurrence of colorectal cancer in a stoma site. Only a few case reports exist in the English literature. The origin of this tumor may be either a metachronous colonic lesion, metastasis to the peristomal skin, or implantation of tumor cells during the initial cancer operation. Both metastatic disease and local recurrence typically present within the first 2 to 4 years after surgery for colorectal cancer.1,2 In previously described case reports, the stoma site cancer was discovered much later (Table 1). Metachronous or synchronous colorectal cancer occurs in 5 to 10% of colorectal cancer cases and are defined as tumors of the colon that do not occur in the anastomotic site and are not suspected for metastasis or extension of other tumors.3
Author | Year of publication | Time from primary resection to recurrence (years) |
| Takami et al 8 | 1983 | 19 |
| Saegusa et al 9 | 1986 | 5 |
| Nakano et al 10 | 1987 | 22 |
| Ohta et al 11 | 1991 | 9 |
| Ishikawa et al 12 | 1994 | 30 |
| Ohtsuka et al 13 | 1996 | 4 |
| Shibuya et al 6 | 1997 | 8 |
| Chintamani et al 5 | 2007 | 6 |
| Chintamani et al 5 | 2007 | 5 |
| Greenberg et al 14 | 2007 | 0.5 |
| Vijayasekar et al 15 | 2008 | 14 |
| Okamoto et al 16 | 2009 | 15 |
| Kuo et al 4 | 2012 | 0.5 |
| Iwamoto et al 17 | 2015 | 27 |
Table 1. Previous case reports of recurrent cancer in colostomy site
In our case report, the fact that the recurrence occurred two years after the initial procedure in combination with the pathology report showing threatened circumferential margins and incomplete total mesorectal excision (TME), increases the likelihood that this is an isolated metastasis. Recurrence at a previous colo-colonic anastomosis is common and is likely due to intraluminal malignant cells that are present at the time of resection and implant the healing anastomotic site. We suspect that malignancy found at a colostomy site may have the same mechanism (implantation of malignant cells at healing site) and therefore suspect that this is more likely a recurrence rather than metachronous malignancy.4 Unfortunately, we do not have genetic testing of either specimen. If on genetic testing the specimens were similar, it would be obvious that this is a recurrence rather than metachronous malignancy.
Stoma site cancer can manifest symptoms such as stoma site bruising, mucosal bleeding, gradual enlargement of the stoma, or stoma site obstruction. Previous case reports describe an extraordinarily long delay in diagnosis due to the slow, progressive nature of the symptoms. Chintamani et al described a case in which the patient presented with stoma obstruction managed with regular finger dilations by his family physician for over one year before a biopsy was performed and the cancer diagnosis was made.5
Shibuya et al also described a case with a delayed diagnosis. The patient had presented multiple times to the local emergency room with symptoms of obstruction. The patient was discharged and treated with manual dilations for over one year. In another case report, the patient suffered from a growing peristomal mass for more than five years until he decided to see a physician. At the time of his initial presentation, the size of the tumor was more than 16 cm at its greatest dimension.6 Our patient presented with complaints of an “enlarging stoma” and peristomal bleeding, which we initially thought was secondary to over granulation and hyperplasia at the edge of the stoma. A biopsy was finally taken, and the diagnosis confirmed only after one year of persistent symptoms.
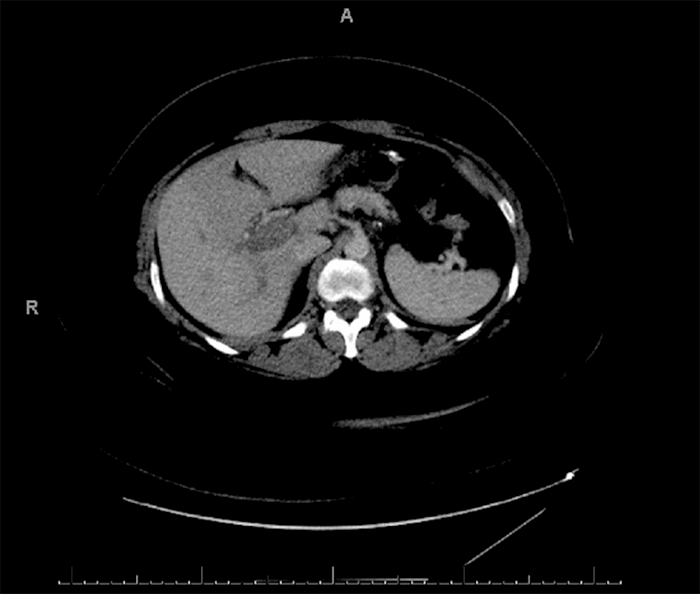
There are no specific guidelines for the treatment of this rare condition and it is our practice to discuss all rectal cancer cases in our multi-disciplinary team (MDT) conference, which is represented by at least one member of each of the following disciplines: surgery, pathology, radiology, medical oncology and radiation oncology.7 Treatment in this case was individualized in accordance with the National Comprehensive Cancer Network (NCCN) guidelines for recurrent rectal cancer to achieve a wide local resection of the stoma including skin, subcutaneous tissues, and the colon with clear margins. Adjuvant chemotherapy will be administered. The surveillance strategy will include history and physical examination with specific focus on inspection of the colostomy, CEA levels and chest/abdomen/pelvis CT every three to six months for the first two years and then every six months for a total of five years. Colonoscopy will be performed at one year after surgery and follow-up colonoscopy will depend on findings.
Conclusion
Rectal cancer recurrence at the colostomy site is extremely rare, as demonstrated by the limited amount of published case reports and supporting literature. Whenever stomal enlargement, persistent bleeding, bruising, or stomal obstructions present, the surgeon must have a high level of suspicion for cancer recurrence. These symptoms should be carefully investigated and there should be a low threshold for stomal mucosal biopsy.
Lessons Learned
Carcinoma in the colostomy site following proctectomy for rectal cancer is rare and mandates a high level of suspicion from the clinician. Possible mechanisms of stoma site carcinoma are recurrence, metachronous malignancy, or metastases. Treatment is based on multi-disciplinary team approach and is patient tailored.
Authors
Shlomo Yellinek, MD
Dimitri Krrizuk, MD
Dan Lavy, MD
Juan J. Nogueras, MD
Correspondence
Juan J. Nogueras, MD
Department of Colorectal Surgery
2950 Cleveland Clinic Blvd.
Weston, FL 33331
Email: noguerj@ccf.org
Presentation
Podium presentation at the annual meeting of the South Florida Chapter of the American College of Surgeons, April 28, 2018, Fort Lauderdale, Florida
Disclosures
The authors have no conflicts of interest to disclose.
References
- Seo SI, Lim SB, Yoon YS, et al. Comparison of recurrence patterns between ≤5 years and >5 years after curative operations in colorectal cancer patients. J Surg Oncol. 2013;108(1):9-13.
- Sargent D, Sobrero A, Grothey A, et al., Evidence for cure by adjuvant therapy in colon cancer: observations based on individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2009;27(6):872-827.
- Moertel CG, Bargen JA, Dockerty MB, Multiple carcinomas of the large intestine: a review of the literature and a study of 261 cases. Gastroenterology. 1958;34(1):85-98.
- Kuo YH, Chin CC, Lee KF, Metastasis at the colostomy site: a rare case report. Jpn J Clin Oncol. 2012;42(8): 753-756.
- Chintamani, Singhal V, Bansal A, Bhatnagar D, Saxena S. Isolated colostomy site recurrence in rectal cancer-two cases with review of literature. World J Surg Oncol. 2007;13(5):52.
- Shibuya T, Uchiyama K, Kokuma M, et al., Metachronous adenocarcinoma occurring at a colostomy site after abdominoperineal resection for rectal carcinoma. J Gastroenterol. 2002;37(5):387-390.
- Richardson, B, Preskitt J, Lichliter W, et al. The effect of multidisciplinary teams for rectal cancer on delivery of care and patient outcome: has the use of multidisciplinary teams for rectal cancer affected the utilization of available resources, proportion of patients meeting the standard of care, and does this translate into changes in patient outcome? Am J Surg. 2016;211(1):46-52.
- Takami M, Hanada M, Kimura M, Takeuchi N, Takada T. Adenocarcinoma arising at a colostomy site. Report of a case. Dis Colon Rectum. 1983;26(1):50-52.
- Saegusa K. A case of recurrent rectal carcinoma in the colostomy site. Chiba Med J. 1986;62:122.
- Nakano H. A case of colon carcinoma revealed by skin infiltration of the colostomy site. J Jpn Surg Assoc. 1987;48:1387.
- Ohta J. A case of metachronous multiple carcinomas arising at a colostomy site after Miles operation. J Jpn Soc Coloproctol. 1991;44:481-484.
- Ishikawa N. A case of carcinoma at the colostomy site 30 years after colon resection. J Jpn Surg Assoc. 1994;55:1603.
- Ohtsuka, M. Treatment of metachronous colorectal cancer that occurred at a stoma after rectum resection because of rectal carcinoma. Surgery. 1996;58:1174–1176.
- Greenberg HL,Lopez L, Butler DF. Peristomal metastatic adenocarcinoma of the rectum. Arch Dermatol. 2006;142(10):1372-1373.
- Vijayasekar C, Noormohamed S, Cheetham MJ. Late recurrence of large peri-stomal metastasis following abdomino-perineal resection of rectal cancer. World J Surg Oncol. 2008;6:96.
- Okamoto N, Maeda K, Hanai T, Sato H et al. Metachronous multiple carcinomas arising at a colostomy site 15 years after abdominoperineal resection: a case report and review of Japanese literature. Int Surg. 2009;94(1):54-57.
- Iwamoto M, Kawada K, Hida K, Hasegawa S, Sakai Y. Adenocarcinoma arising at a colostomy site with inguinal lymph node metastasis: report of a case. Jpn J Clin Oncol. 2015;45(2): 217-220.