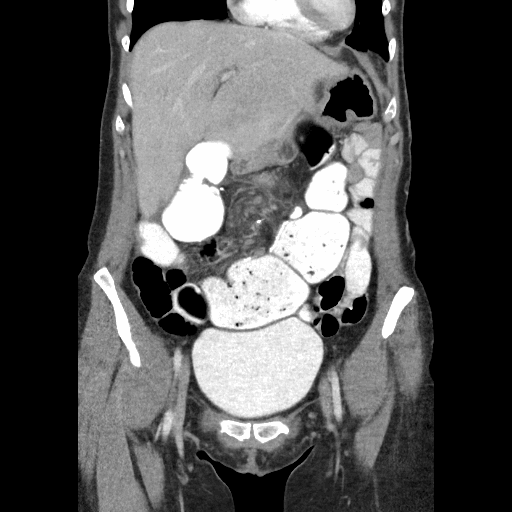
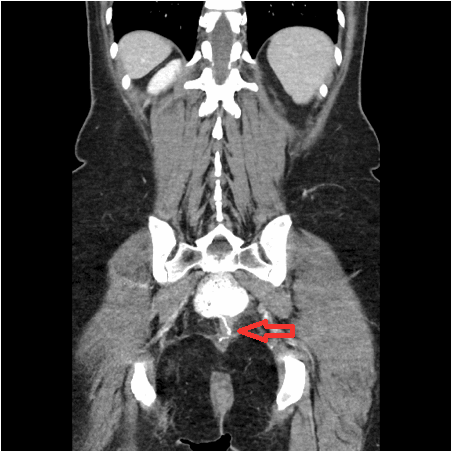
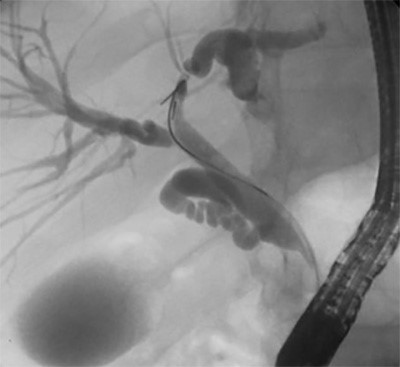
One year later, in July 2018, she began developing similar obstructive symptoms. She had a CT scan (Figure 2 and Figure 3) and underwent a flexible pouchoscopy (Figure 4), which again revealed torsion of the pouch. A red-rubber catheter was inserted into the pouch decompression and temporary relief of symptoms. After a period of bowel rest and resuscitation, she was taken to the operating room for exploration.
Diagnostic laparoscopy confirmed torsion of the pouch, as well as a large internal hernia beneath the mesentery of the J pouch and the retroperitoneum/presacral hollow. All of the old pexy sutures had pulled through. The findings in the operating room at this time were similar to the findings seen one year earlier. The sacral hollow was entirely peritonealized without any adhesions to the pouch. The internal hernia was reduced, which led to complete detorsion of the pouch. An on-table flexible pouchoscopy was performed to ensure no residual torsion was present. The sacral hollow was treated with electrocautery to promote fibrosis and adhesions. A synthetic absorbable mesh was then placed between the sacral hollow and the pouch. Both sides of the pouch were tacked to their respective sidewalls using running barbed sutures, taking bites of the lateral sidewall peritoneum, mesh, and mesentery. The mesenteric defect was closed using the same suture. In addition, a final suture was placed anteriorly to pexy the pouch to the uterus. The postoperative course was uneventful, and the patient was discharged home three days later. At the patient’s five-week postoperative follow-up appointment, she was doing well and had excellent pouch function.
Discussion
For refractory ulcerative colitis, total proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the operative treatment of choice. IPAA is a common procedure used to treat multiple conditions such as ulcerative colitis, certain forms of Crohn disease, indeterminate colitis, and familial adenomatous polyposis. Overall, a patient’s quality of life after the surgery is greatly improved and quite satisfactory, making IPAA the treatment of choice for these conditions.1,2 Unfortunately, there are numerous complications that are unique to patients with an IPAA. Anastomotic leak, abscess, and fistula represent some of the common septic complications, while stricture, pouchitis, and small bowel obstruction are some of the more common nonseptic complications. Prolapse and volvulus of the pouch are some of the rarer complications encountered.2 There have been fewer than twenty cases of pouch volvulus recorded in the literature,5-10 and after an extensive PubMed search, it appears that ours is only the third reported case of a recurrent volvulus.3,4
The first reported case of a recurrent volvulus was published in the literature in July 2014. The patient underwent a standard pouch pexy. This was performed with one row of interrupted non-absorbable monofilament sutures to the presacral fascia. The defect behind the mesentery of the afferent loop was closed with the same type of sutures. However, the patient presented with a recurrent volvulus two months later. On surgical exploration, the previously placed sutures were all detached except for one, similar to the findings in our case. The pouch was untwisted, and two rows of continuous multifilament sutures were placed on either side of the pouch and extended upward in order to close the defect behind the afferent loop of mesentery. The upper corners of the pouch were also sutured to the lateral walls of the pelvis.4
The second case of recurrent volvulus was reported in 2015. This patient presented with a volvulus, and an internal herniation through a mesenteric defect was found. The defect was sutured closed and pouch pexy was performed in a standard fashion. Ten months later, the patient presented again with volvulus and recurrent herniation through a new mesenteric defect. The defect was reduced and closed but pouch pexy was not possible because of the large size of the pouch, which limited access to the sacral hollow and pelvic sidewall. The decision was made to place a rectal tube and four months later the patient returned to have her J pouch revised laparoscopically.3
The majority of reported IPAA volvulus cases have been reported in women with low body mass indexes with the diagnosis of ulcerative colitis who underwent laparoscopic total proctocolectomies with IPAA. The higher incidence in women is thought to be due to the anatomy of a wider pelvis that allows for extra pouch mobility. Low BMI with less adipose tissue in the pelvis is thought to provide more space for pouch torsion. Lastly, it is thought that laparoscopic procedures may lead to increased risk of volvulus due to the paucity of adhesions formed compared to open surgical procedures.8
To our knowledge, our case is only the third reported case of recurrent pouch volvulus after IPAA. It is the only reported case to utilize a laparoscopic approach to recurrent pouch volvulus. It is also unique because it is the first case in the literature to report placement of an absorbable mesh in order to promote adhesion formation behind the pouch.
Conclusion
Pouch volvulus is a rare complication that can lead to significant morbidity. Recurrences are rare. During repair of pouch volvulus, it is important to ensure that the pouch pexy is secure. In addition to a standard sutured pouch pexy to the pelvic sidewall, it may be important to attempt to obliterate the space between pouch mesentery and the sacral hollow, as this is a potential site of small bowel herniation and consequently, retorsion.
Lessons Learned
When treating pouch volvulus, careful attention should be paid to obliterating the space between the sacral promontory, sacral hollow, and the pouch mesentery.
Absorbable mesh can be used to promote adhesion between the sacrum and pouch to prevent recurrent torsion. In our case, a totally absorbable synthetic mesh that is known to cause extensive fibrosis and vascular in-growth was chosen.11
Authors
Gabrielle M. Perrotti, BA
Thomas Jefferson University
Department of Surgery
Philadelphia, PA
Omar Marar, MD
Thomas Jefferson University
Department of Surgery
Philadelphia, PA
Benjamin R. Phillips MD, FACS, FASCRS
Thomas Jefferson University
Department of Surgery
Philadelphia, PA
Correspondence
Gabrielle Perrotti
25 Pollari Circle
Newark, DE 19702
Phone: 302-530-9305
Email: GXP025@Jefferson.edu
Disclosures
The authors have no conflict of interest in terms of the publication of this paper.
References
- Farouk R, Pemberton J, Wolff B, Dozois R, Browning S, Larson D. Functional Outcomes After Ileal Pouch-Anal Anastomosis for Chronic Ulcerative Colitis. Ann Sug. 2000; 231(6): 919-926
- Sherman J, Greenstein AJ. Ileal j pouch complications and surgical solutions: a review. Inflamm Bowel Dis. 2014; 20(9): 1678-85.
- Cardenas G, Bravo R, Delgado S, Jimenez M, Martinez A, Diaz del Gobbo G, De Lacy B, Lacy A.M. Recurrent volvular herniation of the ileal pouch: a case report and literature review. Int J Colorectal Dis. 2016; 31 : 749.
- Myrelid P, Druvefors P, Andersson P. Recurrent Volvulus of an Ileal Pouch Requiring Repeat Pouchopexy: A Lesson Learnt. Case Reports in Surgery. 2014. Volume 2014, Article ID 807640.
- Brady J, Steele S. Laparoscopic Detorsion of an Ileal Pouch and Pouch Pexy. Dis Colon Rectum. 2017; 60: 248.
- Ladisch R, Knechtges P, Otterson M, Ludwig K, Ridolfi T. Pouch volvulus in Patients Having Undergone Restorative Proctocolectomy for Ulcerative Colitis: A Case Series. Dis Colon Rectum. 2018; 61(6): 713-718.
- Mullen MG, Cullen JM, Michaels AD, Hedrick TL, Friel CM. Ileal J-Pouch volvulus Following Total Proctocolectomy for Ulcerative Colitis. J Gastrointest Surg. 2016; 20(5): 1072-3.
- Arima K, Watanabe M, Iwatsuki M, Ida S, Ishimoto T, Nagai Y, Iwagami S, Baba Y, Sakamoto Y, Miyamoto Y, Baba H. Volvulus of an ileal pouch-rectal anastomosis after subtotal colectomy for ulcerative colitis: report of a case. Surg Today. 2014; 44:2382.
- Warren C, O’Donnell ME, Gardiner KR, Irwin T. Successful Management of Ileo-anal Pouch Volvulus. Colorectal Dis. 2011; 13(1): 106-7.
- Jain A, Abbas M, Sekhon H, Rayhanabad J. Volvulus of an ileal J-pouch. Inflamm Bowel Dis. 2010; 16(1): 3-4.
- Yeo KK, Park TH, Park JH, Chang CH, Kim JK, Seo SW. Histologic changes of implanted gore bio-a in an experimental animal model. Biomed Res Int. 2014;2014:167962.