Abstract
Background
A female patient diagnosed with jackhammer esophagus immediately following sleeve gastrectomy.
Summary
A 67-year-old female presented two months postoperatively from laparoscopic sleeve gastrectomy with complaints of nausea, vomiting, regurgitation, dysphagia, and intolerance to both liquids and solids. Initial workup revealed no abnormalities, and observation was recommended. One year later, the patient had no resolution of symptoms and additional testing was performed that showed presbyesophagus, transient reflux, a small hiatal hernia and two small gastric diverticula. Patient underwent further testing prior to consideration for conversion to gastric bypass and was diagnosed with jackhammer esophagus (JE). Calcium channel blocker and proton pump inhibitor (PPI) caused complete resolution of symptoms. While gastroesophageal reflux is a known complication of sleeve gastrectomy, JE is a rare esophageal motility disorder that to our knowledge has not been reported following this procedure. The importance of a thorough workup when a patient presents with reflux symptoms following sleeve gastrectomy prior to conversion to gastric bypass cannot be overstated.
Conclusion
Sleeve gastrectomy is a relatively safe and effective surgery for weight loss. We present a case of JE following sleeve gastrectomy that resolved with calcium channel blocker and PPI. This report highlights the need for a thorough workup in these patients who present postoperatively with reflux type symptoms in order to avoid an unnecessary operation.
Key Words
Sleeve gastrectomy, esophageal dysmotility, jackhammer esophagus, gastroesophageal reflux, GERD
Case Description
Sleeve gastrectomy is a popular option for weight loss surgery1 due to its relative safety and efficacy.2 While there is strong evidence that this procedure affects gastroesophageal motility,2 with gastroesophageal reflux disease (GERD) occurring in about 20 to 30 percent of patients,1 there have been no reported cases of hypercontractile esophageal motility disorders following sleeve gastrectomy. These rare disorders, including jackhammer and hypercontractile esophagus, are thought to be caused by excessive cholinergic or excitatory vagal nerve stimulation causing high amplitude peristaltic contraction.3–5 We report a case of new-onset jackhammer esophagus (JE) after sleeve gastrectomy. The patient had none of the reported symptoms prior to surgery, and her symptoms completely resolved upon starting calcium channel blocker (CCB) and proton pump inhibitor (PPI) medication. To our knowledge, this is the first reported case of JE or hypercontractile esophagus (HE) following sleeve gastrectomy. We will discuss the potential etiology of this condition as well as its pathogenesis as it relates to sleeve gastrectomy.
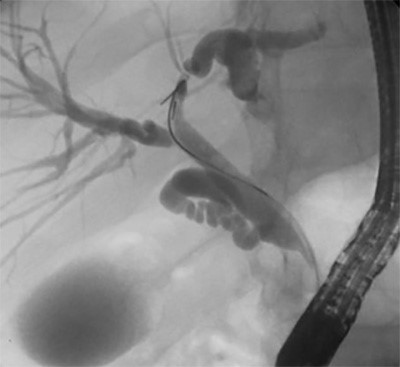
A 67-year-old female underwent a laparoscopic sleeve gastrectomy in October 2016 at a separate institution. Two months later, she was referred to our practice with complaints of incessant nausea, vomiting, regurgitation, dysphagia, and intolerance to both liquids and solids. Initial work-up included upper gastrointestinal endoscopy (UGI) and contrast-enhanced fluoroscopy, both of which revealed normal post-operative findings with no signs of hypermotility, and observation was recommended. One year later, repeat fluoroscopy (Figure 1) performed for persistent symptoms showed presbyesophagus, uncoordinated secondary and tertiary wave contractions with transient reflux, two small gastric diverticula, and a small hiatal hernia.
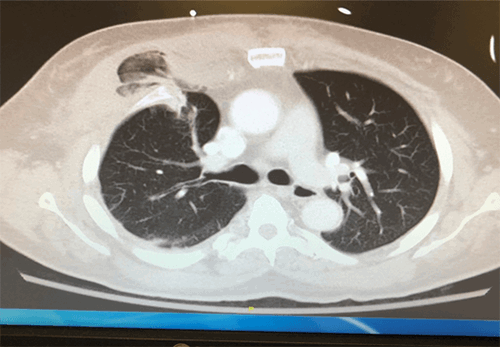
Prior to formally recommending conversion to a gastric bypass, the patient underwent esophageal motility testing. Twenty-four-hour pH testing showed 7.0 percent total acid exposure, symptom association probability >95 percent, and a DeMeester Score of 21.8. Subsequent manometry (Figure 2) showed a hyper-contractile esophagus with four swallows greater than 8000 mm Hg-s-cm, a hypotensive LES, and 100 percent clearance of liquid and viscous swallows. The patient was diagnosed with GERD and JE. She was started on a PPI and diltiazem, and quickly reported resolution of symptoms.
Discussion
Historically, sleeve gastrectomy was the initial procedure in a staged weight loss surgery particularly duodenal switch or Roux-en-Y gastric bypass.3–5 It is currently the most popular weight-loss surgery in the United States and is gaining popularity around the world.6 Sleeve gastrectomy was thought to be mainly a restrictive procedure, but some literature suggests metabolic components of weight loss. Sleeve gastrectomy decreases ghrelin levels,5 an orexigenic hormone,4 and increases gastric emptying causing early satiety. However, sleeve gastrectomy is not without particular complications including bleeding, leak, stricture and GERD.7–9
The patient presented herein had symptoms consistent with GERD and a hiatal hernia, though these are unlikely to cause the extent of dysphagia seen in this case. Thus, our suspicion was high for a new-onset esophageal motility disorder which was confirmed via manometry. JE can present with chest pain, dysphagia, and regurgitation with or without reflux.10 Symptom etiology is not well understood, but esophagogastric junction obstruction has been implicated as a cause of esophageal hyper-contractility following adjustable gastric band placement and fundoplication.10
GERD following sleeve gastrectomy is a common indication for conversion to gastric bypass, but this patient represents a prime example of the importance of a full diagnostic evaluation into other etiologies prior to surgical intervention. This includes upper endoscopy to assess for obstruction, stenosis and esophagitis, 24 hour pH monitoring to confirm a diagnosis of reflux, and high resolution manometry to rule out motility disorders.10,11 The use of dynamic contrast-enhanced fluoroscopy can also be a helpful diagnostic test to visualize the esophagus.10 If a malignant process is suspected, computed tomography and endoscopic ultrasonography may be used for staging purposes.10 The importance of a thorough workup in patients presenting with this constellation of symptoms following a sleeve gastrectomy cannot be overstated. In this case, it avoided an unnecessary surgical procedure.
Our patient experienced prompt resolution of symptoms after being treated with calcium channel blocker medication, a well-established treatment modality for spastic esophageal disorders.10 Calcium channel blockers provide symptom relief by reducing the amplitude of esophageal contractions. Other agents such as anticholinergic agents phosphodiesterase-5 inhibitors,12 nitrates, antidepressants, and even peppermint oil10 are all potentially beneficial medications in the treatment of these disorders. Botulinum toxin injections for spastic esophageal disorders can be considered especially in patients who are experiencing chest pain or have symptoms refractory to oral medications.10 Proton pump inhibitors may also be prescribed in patients with GERD.10
There are several limitation to this case. One being that the index operation for this patient was not performed at our institution and thus her preoperative workup may not have been congruent with our institutional practices. However, the current literature does not support routine UGI or endoscopy in patients undergoing bariatric surgery.13,14 Thus, it is safe to assume that this patient would have been managed preoperatively in a similar fashion.
Conclusion
In conclusion, sleeve gastrectomy affects gastric and esophageal motility in ways that produce both beneficial and adverse effects. We presented a novel incident of JE following sleeve gastrectomy that resolved with calcium channel blocker and PPI therapy. It is important to use caution when assessing patients with reflux symptoms after a sleeve gastrectomy and an extensive evaluation is warranted lest unnecessary surgery be recommended.
Lessons Learned
GERD is a known complication of sleeve gastrectomy that may warrant conversion to gastric bypass. JE is a rare dysmotility disorder that is another potential complication of sleeve gastrectomy. An extensive evaluation is important in the assessment of patients presenting with GERD type symptoms following sleeve gastrectomy.
Authors
Alyssa Green, MD
St. Luke’s University Health Network
Department of Research and Innovation
Bethlehem, PA
Peter Lundberg, MD
St. Luke’s University Health Network
Department of Bariatric Surgery
Allentown, PA
Maher El Chaar, MD
St. Luke’s University Health Network
Department of Bariatric Surgery
Allentown, PA
Correspondence
Primary Author
Maher El Chaar, MD
St. Luke’s University Health Network
Department of Bariatric Surgery
Allentown, PA 18104
E-mail: Maher.ElChaar@sluhn.org
Secondary Author
Alyssa Green, MD
Department of Research and Innovation
801 Ostrum St.
Bethlehem, PA 18015
Phone: 484-526-2240
E-mail: Alyssa.Green@sluhn.org
Disclosures
The authors have no conflicts of interest to disclose.
References
- Amor IB, Debs T, Kassir R, Anty R, Amor VB, Gugenheim J. De novo hiatal hernia of the gastric tube after sleeve gastrectomy. Int J Surg Case Rep. 2015;15:78–80.
- Benaiges D, Mas-Lorenzo A, Goday A, et al. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21:11804–14.
- Bellanger DE, Greenway FL. Laparoscopic Sleeve Gastrectomy, 529 Cases Without a Leak: Short-Term Results and Technical Considerations. Obes Surg. 2011;21:146–50.
- Boza C, Salinas J, Salgado N, et al. Laparoscopic Sleeve Gastrectomy as a Stand-Alone Procedure for Morbid Obesity: Report of 1,000 Cases and 3-Year Follow-Up. Obes Surg. 2012;22:866–71.
- Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 5:469–75.
- Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, Sleeve Dilation, and Barrett's Esophagus after Laparoscopic Sleeve Gastrectomy: Long-Term Follow-Up. Obes Surg. 2017;27:3092–101.
- Sarkhosh K, Birch DW, Sharma A, Karmali S. Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: a surgeon’s guide. Can J Surg. 2013;56:347.
- Brethauer SA. Sleeve gastrectomy. Surg Clin North Am. 2011;91(6):1265–1279.
- Soricelli E, Iossa A, Casella G, Abbatini F, Calì B, Basso N. Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia. Surg Obes Relat Dis. 2013;9:356–61.
- Roman S, Kahrilas PJ. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 2013;42:27–43.
- Martin-Dominguez V, Perez-Fernandez MT, Marinero A, Jusue-Irurita V, Caldas M, Santander C. Hypercontractile esophagus: Clinical context and motors findings in high resolution manometry. Rev Esp Enferm Dig. 2015;107:274–9.
- Hong YS, Min YW, Rhee PL. Two Distinct Types of Hypercontractile Esophagus: Classic and Spastic Jackhammer. Gut Liver. 2016;10:859–63.
- Gómez V, Bhalla R, Heckman MG, et al. Routine screening endoscopy before bariatric surgery: is it necessary? Bariatr Surg Pract Patient Care. 2014;9(4):143–149.
- Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21(S1):S1–S27.