Figure 3. CT scan revealing incarcerated left inguinal hernia with tissue stranding.
The patient was thereafter admitted to the operating room for emergent laparoscopic hernia repair, which confirmed an incarcerated fat containing direct and indirect inguinal hernia. The hernia was reduced laparoscopically with 3D-mesh enforcement. The postoperative period was uneventful, and the patient was discharged home.
Case Description 2
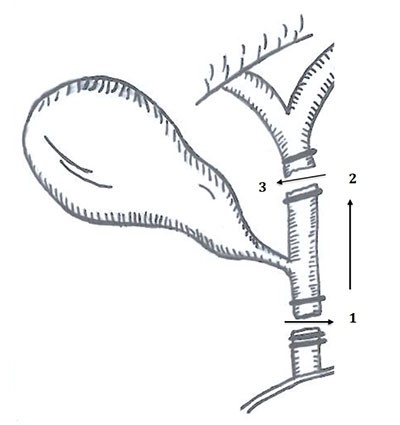
A 48-year-old male with a 20-year history of ulcerative colitis was found to have low-grade adenomatous dysplasia of the rectum. The decision to undergo surgical resection was taken by the patient after discussing the future cancer risk. The patient underwent laparoscopic restorative proctocolectomy with the construction of an ileal J-Pouch anal anastomosis and diverting loop ileostomy.
Postoperatively, clear liquids were advanced to soft diet. However, on postoperative day six, the patient developed abdominal pain, distention, nausea and recurrent episodes of vomiting. A nasogastric tube was inserted, draining 800 cc bilious output. On postoperative day eight, the patient noticed a new tender bulge in the left groin. Physical exam confirmed an incarcerated inguinal hernia.
Open left inguinal hernia repair with intraoperative findings of indirect hernia sac containing necrotic lipoma was identified and excised followed by non-mesh (Bassini) tissue repair. The patient was discharged home on postoperative day one after full recovery.
Discussion
Postoperative ileus is a common complication after abdominal surgery. It is estimated that up to 25.5 percent of hospital readmissions following colorectal surgery are related to a complication of an ileus.5 Prolonged ileus increases the risk of unplanned reoperation by more than three times, prolongs hospital stay, and increases resource utilization. It is estimated that the overall costs of postoperative ileus in the United States can reach up to 1.5 billion dollars annually.6,7
The exact time interval in which physiologic delayed bowel function is differentiated from pathologic postoperative ileus is debatable and poorly defined in the literature.
As suggested by Livingston et al., absence of bowel function on postoperative day three defines the time interval between physiologic and pathologic state.4 However, other reports suggest an ileus longer than six days to be the more appropriate definition of an abnormally prolonged ileus.8
Physiologic postoperative ileus that resolves spontaneously within two to three days reflects inhibition of intestinal motility by hormonal stimulation of alpha II adrenergic reflexes. In contrary, prolonged ileus that lasts more than one week may reflect an underlying undiagnosed postoperative complication that requires further investigation.9
The cause of prolonged postoperative ileus is considered to be multifactorial and involves several technical and physiologic elements. Factors associated with increased risk of postoperative ileus include ASA >2, prolonged operation lasting >3 hours, preoperative sepsis, disseminated cancer, and chronic obstructive pulmonary disease (COPD).11
Multiple studies have demonstrated the benefit of laparoscopic surgery in decreasing the risk of postoperative ileus.6,12,13 Peritoneal violation and mechanical manipulation of the bowel during open procedures stimulates the release of catecholamine, vasoactive intestinal peptides and substance P. Which in turn, generate an inhibitory sympathetic hyperactivity directly inhibiting the myoelectrical activity of the small bowel and the colon. The role of nitric oxide in the pathogenesis of postoperative ileus was suggested in experimental studies however, its deleterious effects in humans remains unclear.14-16
Opioid-based analgesia plays a major role in the management of peri- and postoperative pain after abdominal surgeries. Opioids directly act on cerebral and spinal μ receptors to suppress pain transmission by inhibiting the release of acetylcholine.17 However, the co-stimulation of peripheral μ-opioid receptors found on myenteric and submucosal neurons in the gastrointestinal tract, results in disruptions of the migrating motor complex in the small bowel and decreases the amplitude of propulsive myoelectric waves in the colon. This in turn leads to suppression of excitatory pathways and blocks distention-induced peristaltic contractions delaying return of bowel function.15,18
Patients with prolonged gastrointestinal dysmotility are at higher risk of postoperative complications such as thromboembolic complications, intra-abdominal infections, delayed wound healing and anastomosis leakage.19 Increased morbidity is also associated with the development of nausea and vomiting, which in turn increase the risk of respiratory complications. Tevis et al20 found that up to 60 percent of patients with prolonged postoperative ileus may develop other more severe adverse outcomes after abdominal surgery, suggesting that an ileus may be a precursor to impending poor outcomes.
Similar to the cases we discussed in this report, many patients with an inguinal hernia are asymptomatic. Multiple randomized studies recommend watchful waiting with delayed hernia repair as an acceptable option for patients with minimally symptomatic or asymptomatic inguinal hernias.21,22 However, it is prudent to rule out hernia-related intestinal obstruction in patients with postoperative ileus. A detailed history and physical supplemented by imaging studies is a key element in pinpointing the site of obstruction and differentiating between the two entities. Hernia-related acute small bowel obstruction may present with clinical presentations of abdominal distension, vomiting, nausea, abdominal pain, and distention, all similar to that of postoperative ileus. Hernia-related acute mechanical bowel obstruction is the third leading cause of bowel obstruction,23 with incidence of strangulation, necrosis, and perforation ranging from 6 percent to 24 percent.24,25 Therefore, delay in diagnosis may pose a significant morbidity and worse outcomes.
Discussion
In our report, we presented two cases of incarcerated inguinal hernia occurring in the stetting of postoperative ileus. After review of the literature, we could not find similar complications.
As we emphasize the uniqueness of our cases, we believe that progression of the hernia from being asymptomatic to incarcerated may be related to the postoperative ileus. It is possible that the vomiting and distention directly contributed to increase the size of existing inguinal hernia, leading to incarceration. We believe that increased intra-abdominal pressure associated with vomiting and straining may have forced the hernia contents through the path of least resistance and weakened fascia. Alternatively, the existing hernia could have caused a mechanical small bowel obstruction presenting with similar symptoms of an ileus.
Conclusion
In patients with prolonged postoperative ileus, we strongly recommend further diagnostic investigation to role out an underlying source of mechanical obstruction. Diagnosis of prolonged postoperative ileus should be made clinically. However, additional undiagnosed pathology should be suspected, making an ileus a diagnosis of exclusion. In addition, patients with history of hernia with the potential for incarceration may benefit from preoperative hernia repair prior to a major abdominal procedure, which may decrease the chances of incarceration and further surgical interventions.
Lessons Learned
Postoperative ileus and incarcerated hernia may present with similar symptoms; however, they should not be confused. Preoperative workup with planned elective hernia repair prior to a major abdominal procedure could prevent future incarceration and strangulation of an existing hernia.
Authors
Thaer Obaid, MD
Department of Surgery, Einstein Healthcare Network. Philadelphia, PA
Luanne Force, MD
Department of Colorectal Surgery, Cleveland Clinic Foundation. Weston, FL
Steven D. Wexner, MD, PhD (Hon), FACS, FRCS, FRCS (Ed), FRCSI (Hon)
Department of Colorectal Surgery, Cleveland Clinic Foundation. Weston, FL
Correspondence Author
Dr. Thaer Obaid
Department of Surgery
5501 Old York Rd, Philadelphia, PA 19141
Phone: 215-456-8007
Email: obaidtha@einstein.edu
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Millan M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E. Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg. 2012; 36:179–185.
- Asgeirsson T, El-Badawi KI, Mahmood A, Barletta J, Luchtefeld M, Senagore AJ. Postoperative ileus. it costs more than you expect. J Am Coll Surg. 2010; 210(2):228–31.
- Mattei P, Rombeau JL. Review of the pathophysiology and management of postoperative ileus. World J Surg. 2006;30:1382–1391.
- Livingston EH, Passaro EP. Postoperative ileus. Dig Dis.1990; Sci 35:121–132.
- Lyer S, Saunders WB, Stemkowski S. Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm. 2009;15:485–494.
- Moghadamyeghaneh Z, Hwang GS, Hanna MH, et al. Risk factors for prolonged ileus following colon surgery. Surg Endosc. 2016;30:603–609.
- Goldstein JL, Matuszewski KA, Delaney C, et al. Inpatient economic burden of postoperative ileus associated with abdominal surgery in the United States. P and T. 2007;32:82–90.
- Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, et al. Prolonged Postoperative Ileus—Definition, Risk Factors, and Predictors after Surgery. World J Surg. 2008 Jul;32(7):1495–500.
- Luckey A, Livingston E, Taché Y. Mechanisms and treatment of postoperative ileus. Arch Surg. 2003;138:206–214.
- Millan M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E. Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg. 2012;36:179–185.
- Chapuis PH, Bokey L, Keshava A, et al. Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg. 2013;257(5):909-15.
- Shussman N, Brown MR, Johnson MC, Da Silva G, Wexner SD, Weiss EG. Does nasogastric tube decompression get used less often with laparoscopic and hand-assisted compared with open colectomy? Surg Endosc. 2013;27:4564–4568.
- Böhm B, Milsom JW, Fazio VW. Postoperative intestinal motility following conventional and laparoscopic intestinal surgery. Arch Surg. 1995;130:415–419.
- Kalff JC, Schraut WH, Billiar TR, Simmons RL, Bauer AJ. Role of inducible nitric oxide synthase in postoperative intestinal smooth muscle dysfunction in rodents. Gastroenterology. 2000;118:316–327.
- Luckey A, Livingston E, Taché Y. Mechanisms and Treatment of Postoperative Ileus. Arch Surg. 2003 Feb;138(2):206–14.
- Espat NJ, Cheng G, Kelley MC, Vogel SB, Sninsky CA, Hocking MP. Vasoactive intestinal peptide and substance P receptor antagonists improve postoperative ileus. J Surg Res. 1995;58:719–723.
- Holzer P. Opioid receptors in the gastrointestinal tract. Regul Pept. 2009;155(1–3):11–7.
- Wood JD1, Galligan JJ. Function of opioids in the enteric nervous system. Neurogastroenterol Motil. 2004; Suppl 2:17–28.
- Kronberg U, Kiran RP, Soliman MS, et al. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg. 2011;253:78–81.
- Tevis SE, Carchman EH, Foley EF, Harms BA, Heise CP, Kennedy GD. Postoperative Ileus—More than Just Prolonged Length of Stay? J Gastrointest Surg. 2015 Sep;19(9):1684–90.
- Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomised clinical trial. JAMA. 2006; 295:285–92.
- de Goede B, Wijsmuller AR, van Ramshorst GH, et al. Watchful Waiting Versus Surgery of Mildly Symptomatic or Asymptomatic Inguinal Hernia in Men Aged 50 Years and Older: A Randomized Controlled Trial. Ann Surg. 2018; 267(1):42–49.
- Miller G, Boman J, Shrier I, Gordon PH. Natural history of patients with adhesive small bowel obstruction. Br J Surg. 2000;87:1240–1247.
- Yilmaz A, Gulsen Y, Hasan A. Causes and effective factors on mortality of intestinal obstruction in the South East Anatolia. Turk J Med Sci. 2002;32:149–154.
- Ihedioha U1, Alani A, Modak P, Chong P, O'Dwyer PJ. Hernias are the most common cause of strangulation in patients presenting with small bowel obstruction. Hernia. 2006;10(4):338–40.