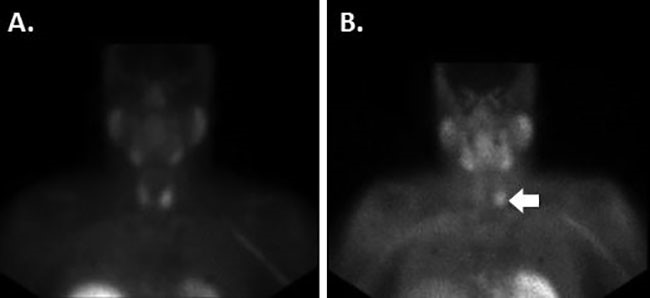
Figure 8. A: Transabdominal preperitoneal dissection (performed to dissect the left obturator hernia sac); B: Obturator hernia sac reduced extraperitoneally; C: The femoral vessels are located lateral to the obturator hernia sac. D: The obturator hernia sac is reduced intraperitoneally.
Discussion
SBO has been recognized since ancient times, going back as far as Praxagoras of Athens, who is credited for performing the first operation for obstruction secondary to strangulated inguinal hernia.1 Hippocrates thought intestinal obstructions did not require surgical therapy.2 It wasn’t until the 1800s and the advancement of anesthesia, antisepsis, and surgical techniques that surgical intervention of intestinal bowel obstruction became accepted. SBO accounts for approximately 12 to 16 percent of surgical admissions, with more than 300,000 operations performed annually at a cost of more than $2.3 billion in the United States.3 While adhesions account for the majority of SBO (60 percent), hernia is the second leading cause (approximately 15 percent).
Both obturator and sciatic hernia are rare pelvic hernias. Obturator hernias account for 0.05 to 1.4 percent of all hernias.4 Sciatic hernias have fewer than 100 cases reported worldwide.5 These rare hernias have high morbidity and mortality due to substantial risk of strangulation; therefore, it is important to understand the pathophysiology, diagnostic methods, and potential treatments. This report presents a rare case where the patient had an SBO due to an obturator hernia and was found to have a concurrent sciatic hernia.
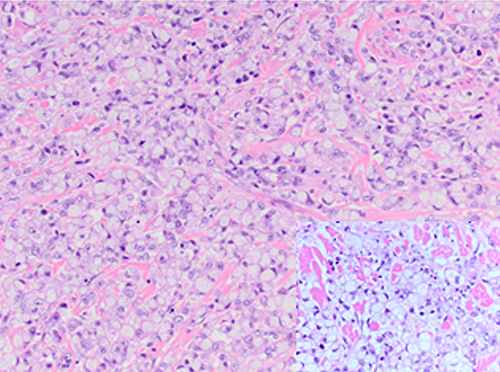
An obturator hernia passes through the canal between the superior ramus of the pubic bone and the obturator membrane and emerges under the pectineal muscle. The obturator canal is about one centimeter wide, contains the obturator nerve and vessels, and is usually covered with preperitoneal fat that prevents hernias from occurring. Obturator hernia accounts for 0.05 to 1.4 percent of all hernias.4 It has a higher prevalence in females due to their wider pelvis and their larger/more triangular obturator canal openings. With greater transverse diameter comes greater space, and thus greater risk.6 Mean age of occurrence is 72.8 years old, and most cases are reported to occur in the seventh or eighth decade of life.6,7 Reports indicate a 6 percent bilateral obturator hernia incidence, though 60 percent of cases occur on the right.4,6 The majority of obturator hernias contain small bowel, but can also contain large bowel/fallopian tube/omentum. Though rare, several risk factors have been identified. Studies have proposed that an obturator hernia can occur due to emaciation, as severe weight loss can cause the loss of the protective preperitoneal fat from the obturator canal. Parity of more than two births has also been identified as a risk factor due to relaxation of pelvic tissue.8 With age or poor nutrition, the loss of preperitoneal fat creates a larger space around the canal, predisposing a herniation into the canal.6 A suggested model of the progression points to three stages: (1) pilot tags of preperitoneal fat can be found in the obturator foramen; (2) the peritoneum forms a dimple before becoming a hernia; (3) abdominal contents enter the hernia.9,10 There is a 57 percent risk of the small intestine’s convex or antimesenteric border to partially protrude or strangulate through this type of hernia.6,11 Specifically, the portion of the small intestine, especially the ileum, that convexly faces away from the root of the mesentery may exacerbate the issue into a Richter hernia, which also has a high mortality up to 11.4 percent.5,6,11 Other proposed risk factors for developing obturator hernia include increased abdominal pressure secondary to chronic obstructive pulmonary disease (COPD), constipation, and kyphoscoliosis.12
A sciatic hernia is herniation through the greater or lesser foramen and may involve small bowel or, rarely, uterus. There are three types of sciatic hernias: suprapiriform muscle (60 percent of cases), infrapiriform (30 percent), and subspinous through lesser sciatic foramen (10 percent). Suprapiriformis sciatic hernia is the most common type, where the hernia protrudes above the piriformis muscle and courses along the superior gluteal artery and nerve. Infrapiriformis sciatic hernia travels with the inferior gluteal vessels, internal pudendal vessels, and the sciatic nerve. Subspinous sciatic hernia leaves the pelvis through the lesser sciatic foramen, medial to the internal pudendal vessels and the sciatic nerve.11 Causes for sciatic hernia are often unknown, but may be related to increased abdominal pressure and/or piriformis muscle atrophy.5 Sciatic hernia can often mimic sciatica due to compression of sciatic nerve.
Patients with obturator and/or sciatic hernia can present with symptoms ranging from asymptomatic to strangulated SBO that causes nausea, vomiting, and abdominal pain. On examination, the commonly discussed Howship-Romberg sign is seen in only 10 to 30 percent of cases: pain in the medial aspect of the thigh caused by compression of the obturator nerve from the hernia, aggravated by extension, abduction and medial rotation, and relieved by flexion of the thigh.12
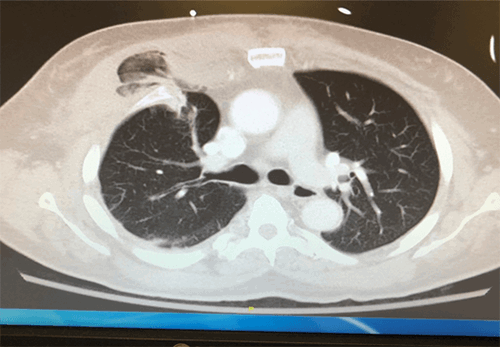
Diagnosing an obturator and/or sciatic hernia by physical exam can be difficult, especially with an obese patient. Diagnosis is commonly obtained through X ray or CT scan. An air-filled bowel loop may be identified in the region of the obturator foramen.12 CT allows accurate identification of the hernia and differentiates from other differentials. Other modalities that may be used include colored Doppler (to check blood flow), bowel viability, and ultrasound. Ultrasound for diagnosis of hernia in the inguinal region was first reported in 1975.12 Ultrasonography may see the hernia sac being represented as a hypo-echoic tubular structure. Ultrasound is noninvasive, but the drawback is that it can be operator-dependent.
Both obturator and sciatic hernia are extremely rare types of abdominal hernia. Obturator hernia has an incidence reported between 0.05 to 1.4 percent based on previous studies.4 Sciatic hernia is even more rare, with less than 100 reported cases.5 The first known report to highlight the two hernias concomitantly was by Dundamadappa et al. published in 2006.12 Karasaki et al. observed that a lower BMI associated with emaciation, pelvic floor muscle atrophy, and loss of preperitoneal fat predisposed patients to pelvic floor hernia.4 It is important to understand that these two types of hernias can potentially cause a Richter-type hernia. Richter-type hernia can frequently result in partial bowel obstruction, delaying diagnosis and causing bowel ischemia, perforation, and severe sepsis, and resulting in higher mortality and morbidity. Therefore, a high index of suspicion is needed.
In this case report, our patient’s age and female gender gives the patient an increased risk of both obturator and sciatic hernia. Our patient was initially managed nonoperatively due to her lack of peritonitis, leukocytosis, and lactic acidosis. The patient was initially treated with nasal gastric tube, bowel rest, and intravenous fluid resuscitation. Due to the lack of improvement in the patient’s obstructive symptoms, the patient was taken to surgery on hospital day two.
Incarcerated symptomatic obturator and sciatic hernia are historically repaired with either an open or laparoscopic approach. Open approach is more commonly used under emergency setting.13 In our case, the obturator hernia was repaired laparoscopically with mesh using transabdominal preperitoneal approach. We elected to use mesh to reinforce the defect since there was no bowel perforation or gangrene encountered during the surgery. The concurrent sciatic hernia was also repaired laparoscopically with high ligation of the hernia sac. There is no consensus on whether to close either obturator or sciatic hernia defects with or without mesh. Simple closure of an obturator hernia defect has a recurrence rate of less than 10 percent.13 Important structures to watch out for during repair include gluteal arteries, pudendal arteries, sciatic nerves, pudendal nerves, and the ureters.
At six month follow-up, the patient has recovered well from the surgery and is asymptomatic of hernia recurrence.
Conclusion
Obturator and sciatic hernia are rare phenomena, but are more commonly seen in patients with emaciation, pelvic floor muscle atrophy, and the loss of preperitoneal fat. This hernia can cause high mortality and morbidity due to the incomplete obstructive nature of the hernia—this can cause a delay in diagnosis. Therefore, both a high index of suspicion in the symptomatic patient and prompt, early surgical repair are important.
Lessons Learned
Obturator and sciatic hernia can occur in patients with emaciation, pelvic floor muscle atrophy, and the loss of preperitoneal fat; therefore, high index of suspicion is important in the symptomatic patient. Prompt, early repair is also necessary, as these hernias can lead to high mortality and morbidity due to their incomplete obstruction nature.
Authors
David W. Chiang, MD
General Surgery Resident, Carle Foundation Hospital, Urbana, Illinois
John H. Kim, DO, MPH, FACS
General Surgery, Trauma Surgery and Simulation Lab Director, Carle Foundation Hospital; Surgery Clerkship Director; Clinical Assistant Professor, Department of Surgery, University of Illinois College of Medicine at Urbana-Champaign
Correspondence Author
Dr. John H. Kim
611 W. Park Street
Urbana, IL 61801
217-383-3240
John.Kim@carle.com
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- Wangensteen OH. Historical aspects of the management of acute intestinal obstruction. Surgery. 1969;65(2):363–83.
- Lohn JW, Austin RC, Winslet MC. Unusual causes of small-bowel obstruction. J R Soc Med. 2000;93(7):365–8.
- Ray NF, Denton WG, Thamer M, Henderson SC, Perry S. Abdominal adhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg. 1998;186(1):1–9.
- Yip AW, AhChong AK, Lam KH. Obturator hernia: a continuing diagnostic challenge. Surgery. 1993;113(3):266–9.
- Karasaki T, Nakagawa T, Tanaka N. Sciatic hernia: is it really rare? Surg Today. 2014;44(6):1079–83.
- Thanapaisan C, Thanapaisal C. Sixty-one cases of obturator hernia in Chiangrai Regional Hospital: retrospective study. J Med Assoc Thai. 2006;89(12):2081–5.
- Wakeley C, Wakeley J. Rare types of external abdominal hernias. In: Schwartz SI, Ellis H, Husser WC, editors. Maingot’s abdominal operations. Norwalk Ct: Appleton & Lange, 1989.
- Bjork KJ, Mucha P Jr, Cahill DR. Obturator hernia. Surg Gynecol Obstet. 1988;167(3):217–22.
- Franklin RH. Obturator hernia. Lancet. 1938;1:721–2.
- Singer R, Leary PM, Hofmeyr NG. Obturator hernia. S Afr Med J. 1955;29(4):73–5.
- Cali RL, Pitsch RM, Blatchford GJ, Thorson A, Christensen MA. Rare pelvic floor hernias. Report of a case and review of the literature. Dis Colon Rectum. 1992;35(6):604–12.
- Dundamadappa SK, Tsou IY, Goh JS. Clinics in diagnostic imaging (107).Singapore Med J. 2006;47(1):89–94.
- Siow SL, Voon KKT. Two different surgical approaches for strangulated obturator hernias. Malays J Med Sci. 2012:19(1): 69–72.