Bibliography
American College of Surgeons. Dateline DC—STOP THE BLEED demonstrates how advocacy has the power to effect change. Bull Am Coll Surg. June 1, 2019. Available at: https://bulletin.facs.org/2019/06/dateline-dc-stop- the-bleed-demonstrates-how-advocacy-has-the-power-to-effect-change. Accessed September 5, 2021.
Bulger EM, Kuhls DA, Campbell BT, et al. Proceedings from the Medical Summit on Firearm Injury Prevention: A public health approach to reduce death and disability in the US. J Am Coll Surg. 2019 Oct;229(4):415-430.
Bulger EM, Rasmussen TE, Jurkovich GJ, et al. Implementation of a National Trauma Research Action Plan (NTRAP). J Trauma Acute Care Surg. 2018;84(6):1012-1016.
Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):163-173.
Carrico JC. In Search of a Voice. Bull Am Coll Surg. 1999;84(5):14-22.
Dicker RA, Thomas A, Bulger EM, et al; ISAVE Workgroup; Members of the ISAVE Workgroup. Strategies for Trauma Centers to Address the Root Causes of Violence: Recommendations from the Improving Social Determinants to Attenuate Violence (ISAVE) Workgroup of the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2021 Sep;233(3):471-478.
Jacobs LM, McSwain NE, Rotondo MF, et al. Improving survival from active shooter events: The Hartford Consensus. J Trauma Acute Care Surg. 2013;74(6):1399-1400.
Jacobs LM. Implementation of The Hartford Consensus initiative to increase survival from active shooter and intentional mass casualty events and to enhance the resilience of citizens. Bull Am Coll Surg. 2015;100(1Suppl):83-86.
Jacobs LM, Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass-Casualty and Active Shooter Events. The Hartford Consensus III: Implementation of Bleeding Control: If you see something do something. Bull Am Coll Surg. 2015;100(7):20-26.
National Academies of Science, Engineering, and Medicine. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Washington, DC: The National Academies Press; 2016.
Price MA, Kozar RA, Bulger EM, et al. Building the future for national trauma research. Trauma Surg Acute Care Open. 2020;5(1):e000421.
Rasmussen TE. A national trauma care system: From call to action. J Trauma Acute Care Surg. 2016;81(5):813-815.
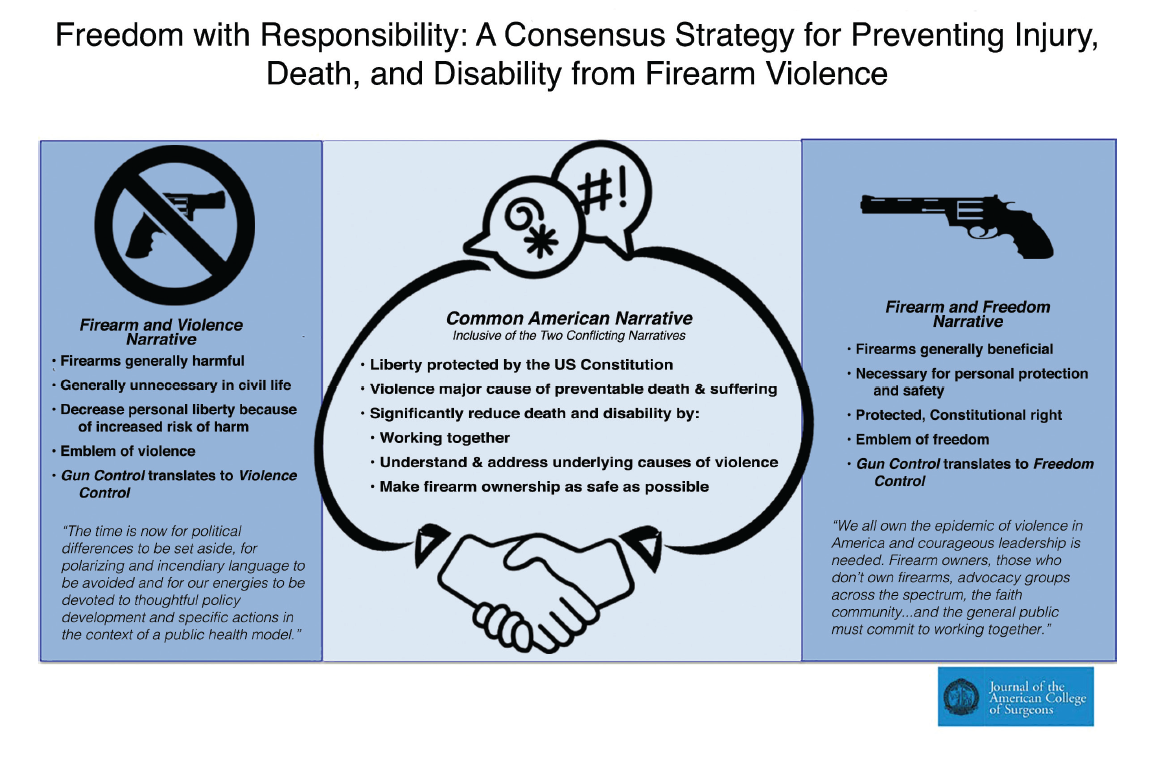
Stewart RM, Kuhls DA, Rotondo MF, Bulger EM. Freedom with Responsibility: A Consensus Strategy for Preventing Injury, Death, and Disability from Firearm Violence. J Am Coll Surg. 2018 Aug;227(2):281-283.
Talley CL, Campbell BT, Jenkins DH, et al. Recommendations from the American College of Surgeons Committee on Trauma’s Firearm Strategy Team (FAST) Workgroup: Chicago Consensus I. J Am Coll Surg. 2019 Feb;228(2):198-206.
Winchell RJ, Eastridge BJ, Moore MM, et al. Developing a national trauma system: Proposed governance and essential elements. J Trauma Acute Care Surg. 2018;85(3):637-641.