Dr. Salminen also is the lead investigator of the Appendicitis Acuta (APPAC) randomized trials, which focus on the treatment of uncomplicated acute appendicitis.
“The main point I want everybody to internalize is the fact that we are talking about two very different diseases,” explained Dr. Salminen. “After you decide that the patient has acute appendicitis, you have to figure out whether it’s the milder form, which is approximately 60% to 70% of cases, or if it is the more difficult form.” She said a primary goal of the inclusion criteria for the APPAC trials (and also clinically) was to rule out patients with complicated acute appendicitis.
Evidence for Antibiotics
The three APPAC trials function as a continuation of research stemming from the initial trial that compared nonoperative management with appendectomy in adults with CT-verified uncomplicated acute appendicitis.
The 5-year follow-up of the first trial (November 2009 to June 2012 in Finland) was completed in September 2017. Among the 530 patients who were selected for the randomized clinical trial, 257 individuals were in the antibiotics group. At the 1-year mark, 70 patients in the group received an appendectomy, with 30 additional patients requiring the procedure between 1 and 5 years.4 The cumulative recurrence rate evaluated by appendectomy mandated by the study protocol for suspected recurrence was 34% at 2 years, 35.2% at 3 years, 37.1% at 4 years, and 39.1% at 5 years.2
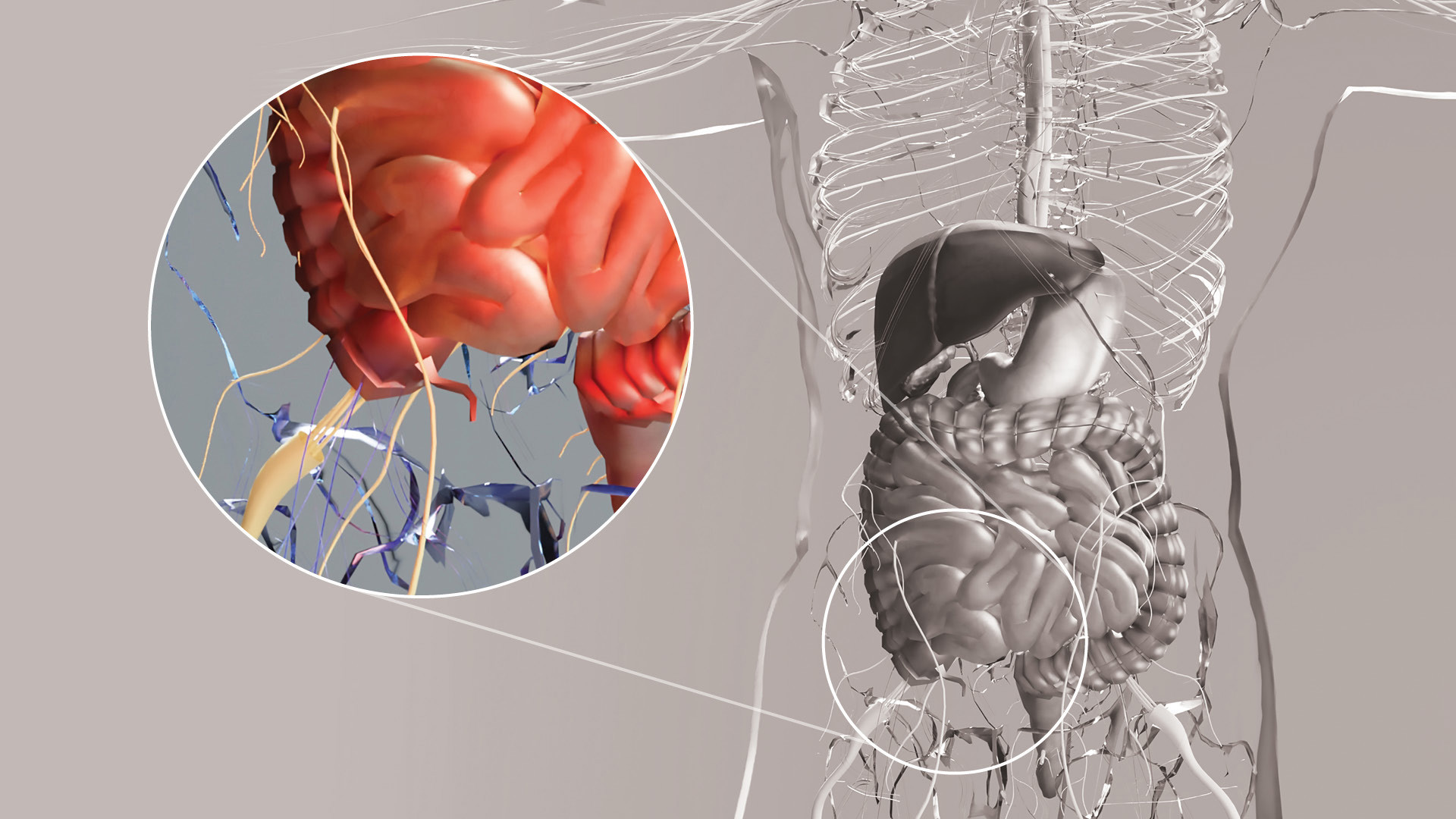
“Surgery is always a big deal, and everything we do carries risk,” said Drew Gunnells Jr., MD, FACS, assistant professor in the Division of Gastrointestinal Surgery at The University of Alabama at Birmingham. “Although an appendectomy is one of the more straightforward procedures we do, there's still risk associated with it. And, so, can we avoid surgical intervention for a disease that for a long time has been treated with surgery?”
According to Dr. Gunnells, as long as the chance for the patient with uncomplicated appendicitis requiring an operation in the future is minimal, treatment with antibiotics may be a safe option. “I think, based on the Comparison of Outcomes of Antibiotic Drugs and Appendectomy (CODA) trials and the APPAC trials, you’re not putting the patients at risk of undue harm by treating them with antibiotics. The question in my mind is: What's the recurrence rate of appendicitis, and are those patients going to need surgery in the future?”
CODA, a large, randomized clinical trial of antibiotics for appendicitis, was conducted at 25 US medical centers. From May 2016 to February 2020, 1,552 adults with appendicitis were randomly assigned to receive either antibiotics or appendectomies. According to findings presented at ACS Clinical Congress 2020 and published simultaneously in The New England Journal of Medicine, approximately half of the patients in the trial did not require an appendectomy up to 4 years after receiving antibiotics.5
Despite these findings, clinicians are encouraged to review the data with a critical eye. “We need to have an evidence-based approach to treating uncomplicated appendicitis and not an eminence-based approach,” suggested Dr. Salminen, underscoring the importance of carefully assessing new and existing research in this area.